筆記目錄
這篇文章提供了完整的食藥署 LDTs 精準醫療分子檢測實驗室認證申請指南,涵蓋申請對象、流程、費用、人員資格、審查時程及後續管理等重要內容,並在本文最後附上《精準醫療分子檢測實驗室檢測與服務指引符合性查核基準》完整原文與 ISO 15189:2012 對照內容。
本攻略只適用於「特定實驗室」。依《特定醫療技術檢查檢驗醫療儀器施行或使用管理辦法》(特管辦法)第 2 條,「特定實驗室」的定義是:「由『非』醫療機構設立,經中央主管機關許可,提供實驗室開發檢測之實驗室。」白話說,就是通過食藥署的特定檢驗實驗室開發檢測認證(精準醫療分子檢測實驗室認證)的業界實驗室,而非醫療機構內設立的實驗室。
關鍵摘要
誰需要申請?
- 本篇文章只適用於非醫療機構所設立的「特定實驗室」。
- 申請前須確認檢測技術、項目、目標族群是否納入食藥署規範。
申請流程
實驗室認證(第一階段)
- 向食藥署申請「精準醫療分子檢測實驗室認證」。
- 涵蓋 QMS(品質管理系統) 建置,向食藥署申請遞件,食藥署進行書面審查、實地查核、專家評估與諮詢會議等。
施行計畫(第二階段)
- 需與醫療機構合作,由醫療機構向醫事司提交「LDTs 施行計畫」。
- 經審核通過,才能正式向民眾提供 LDTs 檢測服務。
關鍵條件
人員資格:至少 2 位醫事檢驗師 擔任「專任品質主管」與「專任技術人員」,並完成專業訓練取得證書。
費用:申請費 40,000 + 每檢測項目 60,000 新台幣。
時程:從申請到核准約需 9 ~ 12 個月。
後續管理:通過認證後需每年 3 月 1 日前提交前一年度的「實驗室間比對方案」報告,並每 3 年申請展延。
注意事項
LDTs 只能與醫療機構合作,不能直接對病患提供檢測。並且,審查過程繁瑣,涉及多次補件,(體感上)送件後的流程,與醫材法規相比更為繁瑣耗時。
本攻略包含初步評估 → 申請準備 → 送件審查 → 認證核准的全流程,希望中小型生技公司與新創實驗室也能順利獲得認證 (ง๑ •̀_•́)ง
1. 前言
因為在人生道路上繞了點路,消失了好久。回來後,誤打誤撞跑到了(似乎充滿政治角力的)實驗室開發檢測技術的產業(Laboratory Developed Tests,LDTs),開始了一段充滿了特殊體驗的旅程。

到職前,公司內有人跟我說:「我們公司已經有資深法規人員建立了一半 QMS 了。」當時不以為意,後來也忘光光。到職後某天和大老闆閒聊:「我們之前已經有一半的 QMS 了,所以應該很快就可以取證吧。」老闆如是說。
我心頭一驚 (☉д⊙)!因為明明就什麼都沒有呀!問了傳說中的「資深法規」,他說:「很抱歉讓你有這個困擾,我當時是跟老闆們說『如果有模板的話,可以省一半的時間』。」
但實際情況是,啥都沒。
我該跑去和老闆們說他們聽錯了嗎?無論我該不該,我當時就摸摸鼻子,悶著頭趕快把網路上能找到的資料全部收集起來,盡快了解什麼是 LDTs?認證流程是什麼?依循的標準是什麼?
在找完資料後才發現,原來我不小心踏入了很久以前,我以為和我沒關係的「獨厚醫技,排外生技」的領域。後來也參加了幾場研討會,對於有勁基因的經驗分享印象深刻,分享人說:「實驗室稽核時,來的都是醫檢師背景,很明顯感受到對於生技、生科背景的敵視。」(不過我自己沒有感受到啦~)
快轉至今,一年過去了,食藥署的精準醫療分子檢測實驗室認證已接近完成,就來分享一下我的金魚腦內僅剩的記憶吧。
嗨,大家!有沒有人的公司有計畫申請食藥署的 LDTs 實驗室認證呢?如果你們公司人數少於 20 人,沒有專門的 RAQA 編制,極度不熟悉《精準醫療分子檢測實驗室檢測與服務指引符合性查核基準》(Backup)在說啥,感覺實驗室認證前途茫茫的話,歡迎寄 email 給我,我很樂意和各位深度交流,甚至一起建立 LDTs QMS,因為其實滿好玩的啊 (*‘ v`*)
2. 開始前,確認是否需要申請 LDTs 認證
如同醫療器材上市路徑的第一步是確認產品的「分類(是不是醫療器材)」與「分級(風險等級是什麼)」,在走上 LDTs 實驗室認證旅程前,也要先確認自己的技術 / 服務是否需要申請 LDTs 認證。
《特管辦法》第 7 條規定:
醫療機構施行第三章第二節所定特定檢查、檢驗之實驗室開發檢測項目,應檢具下列文件、資料,向中央主管機關申請核准後,經直轄市、縣(市)主管機關登記,始得為之:
一、專任品質主管、專任技術人員及核發檢測報告人員之醫事人員證書及專業訓練證明。
二、專任檢測開發、分析、校正、生物資訊處理及其他相關人員之專業訓練證明。
三、第三十六條所定施行計畫。
四、第三十七條認證實驗室合格證明。
而第 36 條說,關於哪些 LDTs 要遵循《特管辦法》是規定於附表四(Backup)。不過看了附表四,也只有寫哪些檢測項目(目的)要被列管,卻沒說哪些技術會被列管。難道是無論是用什麼技術,只要符合《特管辦法》附表四的檢測項目(目的)都會被納管嗎?
當然不是!
目前在衛福部實驗室開發檢測官網或食藥署精準醫療分子檢測實驗室認證(列冊登錄)專區上,只能看到《醫療機構施行實驗室開發檢測項目申請須知》(Backup)的附件一有「實驗室開發檢測項目分類表」:
| 檢測項目類別 | 第一類 | 第二類 | 第三類 |
|---|---|---|---|
| 使用之檢測技術名稱 | 1. 次世代定序(Next generation sequencing,NGS) 2. 微陣列晶片(Microarray) 3. 基因表達譜(Gene expression profiling) | 1. 基因擴增(Gene amplification) (1)聚合酶連鎖反應(Polymerase chain reaction,PCR)+ 膠體電泳(Gel electrophoresis) (2)反轉錄酶連鎖反應(Reverse ranscriptase polymerase chain reaction,RT-PCR) (3)巢式聚合酶連鎖反應(Nested polymerase chain reaction,Nested PCR) (4)三核苷酸重複序列分析(Triplet repeat primed polymerase chain reaction,TP-PCR) (5)短串聯重複序列分析(Short-tandem-repeat analysis) (6)多重聚合酶連鎖反應(Multiplex polymerase chain reaction,Multiplex PCR) (7)等位基因特異性聚合酶連鎖反應(Allele-specific polymerase chain reaction,ASPCR) (8)微滴式數字聚合酶連鎖反應(Droplet digital polymerase chain reaction,DD-PCR) (9)基因甲基化分析(Bisulfite polymerase chain reaction,Bisulfite PCR) (10)序列特異性聚合酶連鎖反應(Sequence specific primers PCR,SSP PCR) (11)多重連接探針擴增技術(Multiplex ligation-dependent probe amplification,MLPA) (12)序列特異性寡核酸法(Sequence-specific oligonucleotides probes)/ 等位基因特異性寡核甘酸雜交(Allele-specific oligonucleotide hybridization) (13)限制性片段長度多態性(Restriction fragment length polymorphism,RFLP) 2. 即時偵測基因擴增(Real-time polymerase chain reaction,Real time PCR) 3. 桑格氏定序(Dideoxy chain-termination method / Sanger method) 4. 焦磷酸定序(Pyrosequencing) 5. 變性高效能液相層析(Denaturing high performance liquid chromatography,DHPLC) 6. 質譜分析(Mass spectrometry analysis)/ 基質輔助激光解吸電-飛行時間質譜(Matrix-assisted laser desorptionionization-time of flight mass spectrometry,MALDI-TOF MS) | 1. 螢光原位雜交技術(Fluorescence in situ hybridization,FISH) 2. 染色體核型分析(Karyotype analysis) 3. 南方墨點法(Southern blot) |
綜合《特管辦法》附表四(Backup)與上述「實驗室開發檢測項目分類表」,並且請教估狗大神後,找到了食藥署《精準醫療分子檢測實驗室認證相關規範說明》和《精準醫療分子檢測實驗室檢測與服務指引》才確認,只有當「檢測技術分類」及「檢測項目分類」都落在「申請條件」內的檢測服務,才會被納管:

後來又聽到一種說法:「只要檢測技術的目標族群是『健康及亞健康』的人,即使檢測技術分類和檢測項目分類均符合申請條件,也不會被納入管制。」如果檢測服務不受《特管辦法》管制,就不用擔心這篇文章內一堆繁雜的規定,可以直接在醫療機構、健檢中心或任何想要的地方提供服務。
上述說法的可能理由是:《特管辦法》第 2 條第六款:「實驗室開發檢測:指為診察、診斷或治療特定病人或疾病之目的,由認證實驗室自行建立及使用之檢測。」
不過,一個檢測技術就算只給健康及亞健康族群做,也可以算是診察「特定疾病」吧?例如,一個自以為健康的人去醫院,說我要確認我有沒有 X 癌,這時候醫生就拿出 A 檢測服務去檢查,檢查結果顯示這個人有沒有 X 癌。這樣不算是診察特定疾病嗎?我們不是常常在做這類事情嗎?
為什麼沒有官方文件明確說明,只有當檢測服務的「檢測技術分類」、「檢測項目分類」和「目標族群」都符合規定,才會被《特管辦法》列管為 LDTs?
誤入 LDTs 領域後,覺得就像是在蠻荒時代,一堆傳聞、聽說…連這麼基本且重要的問題,也沒有明確的解釋與答案,一切都是 case by case,交由那些專家委員決定。「你們要給我們明確的服務規格,我們的專家委員才會判定啊!」從頭到尾都是這種感覺。甚至,連屬性判定要繳交哪些資料都沒有訂出來呢!我還曾經在屬性判定時,被要求要給確效資料!蛤?要確欸!屬性判定時,產品就必須已經開發完,然後要給得出確效報告了喔 (-`ェ´-╬)?
抱怨一下!不知道為什麼他們會搞得那麼複雜,是想說因為「檢測技術」可能會比「檢測項目」更新頻繁,所以不寫在《特管辦法》中比較好修改嗎?但至少也要在食藥署或衛福部官網公布完整一點的指引嘛!不要各種資訊散落在不同的公告、指引、說明會投影片中。其實目前 LDTs 也就那一丁點資訊,沒什麼內容好公布,全部資訊可以整理成少少幾份完整指引,然後官網一直改版相同的文件就好了嘛!
另外為什麼他們公布的須知、基準等等的 PDF 檔,常常無法正常搜尋內容,也無法完整複製內容呢?
實在很想幫他們統整資訊欸 ┏( .-. ┏ ) ┓
3. 要準備多少錢
一、國內實驗室初次認證,或認證事項新增:
(一)申請費:每一申請案新臺幣四萬元。
(二)實地查核費:每一檢測項目新臺幣六萬元。
三、國內實驗室之認證變更申請費:新臺幣二萬元;僅涉及實驗室(或機構)之名稱、負責人、品質主管或檢測名稱之變更,新臺幣五千元。
所以,就是「40,000 + 60,000*檢測項目 = 申請總費用」
4. 最重要的事:人員資格
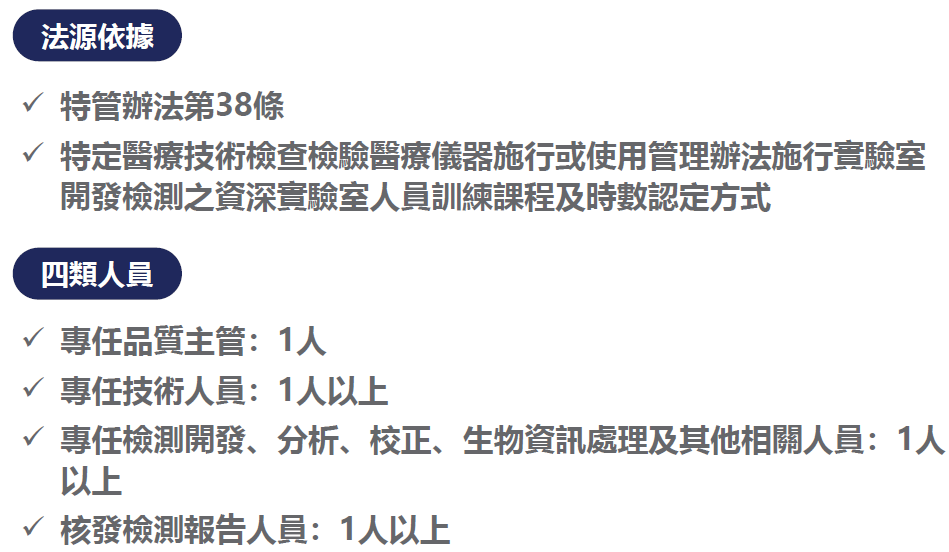
如我前面說的,實驗室開發檢測領域(LDTs)似乎是政治角力的結果。如果去上「實驗室開發檢測之實驗室人員訓練課程」,可以聽到醫技系老師在課堂上一直說:「現在沒人要讀醫技系了。」兩天的授課講師,除了資安老師、生物資訊老師、醫師外,其他都是醫技系的老師。以下是《特管辦法》第 38 條的人員資格,更可以看出獨厚(?)醫檢師的結果:
1. 醫療機構施行實驗室開發檢測,應由自行設置或委託認證實驗室為之;其委託認證實驗室為之者,該受託實驗室應置下列人員:
一、專任品質主管:一人,具醫事檢驗師或專科醫師資格,且有臨床檢驗品質管理及相關實驗室開發檢測經驗二年以上。
二、專任技術人員:一人以上,且具醫事檢驗師資格,並完成中央主管機關公告之訓練課程及時數,取得訓練單位發給之證明。
三、專任檢測開發、分析、校正、生物資訊處理及其他相關人員:一人以上,完成中央主管機關公告之訓練課程及時數,取得訓練單位發給之證明。
四、核發檢測報告人員:一人以上,經相關訓練之醫事檢驗師或專科醫師,並得由第一款、第二款人員擔任。
2. 前條第五項境外實驗室,其前項第二款、第三款人員之資格及訓練,得由中央主管機關認定,不受前項規定之限制。

(上述四項人員資格規定中,有三項必須是「醫事檢驗師」或醫師。如果單純規定是醫師,那合情合理(但不一定可行)。LDTs 產業中,很多是用學校實驗室常用的生物技術,例如 NGS(Next Generation Sequencing)搭配生物資訊來得到結果。以操作、應用技術,以及解讀結果的角度來說,生技背景的人應該不會比醫事檢驗師遜色多少。另外,有多少醫檢師擅長品質管理?在 2024/09/06 的《醫療機構施行實驗室開發檢測項目-申請及審查流程說明》(pg.39)中說明「相關實驗室開發檢測經驗 2 年以上」就可以當品質主管。做實驗的人一定懂品質系統、品質管理?如果真的人員證書、經驗會影響 LDTs 品質那麼多,那就應該不只要求有醫檢師資格就好,應該也要「嚴格」規定有多少年的「直接且實際」的相關經驗。
另外,既然都制訂這些人員資格規定了,既然都說很在意病人安全和醫療品質,那就來嚴格稽核是否有非醫檢師或非醫師的人員違反規定去操作技術人員的工作,是否有在例行檢驗中去操作到檢體或檢體後續的衍生物嘛!但現在實際情況是,相關政府機關並沒有很嚴格要求實驗室例行作業時要遵守人員資格規定,只有在文件審查時要看到實驗室有聘足量的醫檢師罷了。
不過如果真要像我說的那樣搞,可能會關掉很多公司吧 ╮(╯_╰)╭
醫檢師有醫事檢驗師公會,生技系畢業生則什麼都沒有。就像藥師公會之前要「醫藥分業」,現在想要取走獸醫的「動物使用人藥」調劑權一樣,醫檢師公會當然也要卯起來搶走 LDTs 這塊「小餅」,企圖增加醫技系的就學率、畢業生薪資及工作機會(?)
上述《特管辦法》第 38 條中,只剩下第三類人員可以讓「非醫事檢驗師」擔任。如果生物資訊人員強制只能由醫檢師或醫師擔任,那想當然知道 LDTs 在台灣就做不下去了(或者變成一堆掛牌?)。猜測是因為如此,所以第 38 條才有了第三類人員資格。同時又為了要表現出「沒有獨厚醫檢師,還是有重視生技人的專業」,所以第 38 條中還有其他的「雜魚」角色,像是檢測開發人員,或不知在幹嘛的「其他」人員。
(寫在 §38 裡面的人,都要去上滿一定時數的課程,但「其他人員」一定要嗎?例如:業務、採購、人資很重要,但他們沒去上課會怎樣嗎?不會。既然這些重要的「其他人員」不用上課,那寫進 §38 做什麼呢?另外,現在台灣的 LDTs 規定《精準醫療分子檢測實驗室檢測與服務指引符合性查核基準》不要求 Design control,可以憑空就蹦出一個 LDTs,根本沒 Design History File(DHF),那要「檢測開發人員」幹嘛?有什麼地方是只有這類人可以簽核,但其他人不行嗎?並沒有嘛。)
因為專任品質主管、專任技術人員必須由「專任」醫檢師擔任,所以,公司至少要找到「兩名」醫檢師才行,而這兩位都可以「兼任」核發檢測報告人員,而「三、專任檢測開發、分析、校正、生物資訊處理及其他相關人員」也是要一名人員專任,但不要求是醫檢師了。

舉例來說明「專任」和「兼任」的差別:
1. A 醫檢師擔任「專任」品質主管,則 A 就不可以再擔任「專任」技術人員,但可以擔任「兼任」技術人員,以及「兼任」核發檢測報告人員。
2. B 醫檢師如果已經是「專任」技術人員了,還可以當「專任」品質主管和「專任」核發檢測報告人員嗎?不行,但可以當「兼任」核發檢測報告人員。
所以,《特管辦法》第 38 條規範下,一個實驗室至少要有兩名醫檢師,分別擔任「專任」品質主管,以及「專任」技術人員。

另外,為了符合《特定醫療技術檢查檢驗醫療儀器施行或使用管理辦法施行實驗室開發檢測之實驗室人員訓練課程時數採認及課程辦理須知》關於實驗室人員訓練課程時數的規定,第 38 條內的人都必須上滿一定時數的「實驗室開發檢測之實驗室人員訓練課程」,而這門課一年可能就開兩場,一場是上半年(可能 3 月),下半年(可能是 11 月)開另一場,錯過就要再等半年。
所以,才會說人員資格很重要 ┐(´д`)┌
對《特管辦法》第 38 條「爭取」歷史有興趣的筆友,可以到社團法人中華民國醫事檢驗師公會全國聯合會查看「特管辦法LDTs人員資格」(Backup) 的公告。
5. 審查流程及預計時程
這部分不止講第一階段的食藥署「精準醫療分子檢測實驗室認證」,還包括第二階段醫事司的「實驗室開發檢測施行計畫」審查。


5.1 流程摘要
Step 1. 實驗室認證(第一階段):一般業界實驗室向食藥署申請認證,目標成為「特定實驗室」。(主管機關:食藥署)
Step 2. 合作醫療機構(準備第二階段):尋找並確定願意合作的醫療機構。
Step 3. 提交施行計畫(第二階段):醫療機構向醫事司提交「實驗室開發檢測施行計畫」。(主管機關:醫事司)
Step 4. 計畫審核(第二階段):醫事司審核施行計畫,核准後進入 Step 5,未核准則修正後重新提交。(主管機關:醫事司)
Step 5. 地方登記:在地方主管機關完成登記手續。(主管機關:衛生局)
Step 6. 提供服務:經由醫療機構,正式向民眾提供 LDTs 服務。

以下提供兩張精準醫療分子檢測實驗室認證流程圖(也就是上述的 Step 1)供大家參考:

上圖節錄自《精準醫療分子檢測實驗室認證申請須知》的「附件二、認證審查流程圖」。這份《申請須知》只能用 TFDA 全站搜尋或估狗找到,但在「精準醫療分子檢測實驗室認證(列冊登錄) 專區」裡面是找不到的。
整個食藥署精準醫療分子檢測實驗室認證非~常繁瑣 (〒︿〒)!以下是我的抱怨,可以完全跳過不看。
首先,在遞件後,食藥署會進行形式審查,並要求補件及繳費。一直到這裡都沒什麼問題。
接下來,申請案就轉交給 TAF,書面審查有可能會被要求補件兩次,並且「不能」直接和審查員溝通,就只能看著補件通知憑感覺隔空抓藥。這是非常沒效率的規劃,很多問題可能只要跟審查員溝通幾分鐘就可能不用補件、修改,或者可以很有效率地釐清問題後,針對問題補件,但因為「無法跟審查員溝通」的規定,導致必須曠日廢時來回兩次。
再來就是實地查核。
實地查核後,又可能會需要補件兩次。(我又忍不住把 LDTs 的流程跟醫療器材相比,明明人家醫療器材風險等級比 LDTs 高,但 LDTs 這個階段要補件兩次?)
接著,在進入最後的專家諮詢會議之前,申請案會轉交給「另外」的審查員(不同於書面審查和實地查核的審查員),這時「又」會被問問題,「又」要補件。
這樣的流程設計,是代表食藥署很不信任書面審查、實地稽核的審查員,才要找另外兩位專家審查嗎?這兩位「新出現」的專家過去又沒有跟我們討論過,他們只是看著我們「非最新版」的書面資料,就要開出補件通知。然後,我們一樣不能和開出缺失的專家確認問題是什麼,一樣要隔空抓藥回覆缺失。
(和醫療器材的上市流程(QMS 認證 + 查驗登記)比起來,LDTs 的流程真的冏。)
接著,申請案就轉回去食藥署,進入專家諮詢會議。
原本以為已經被那麼多人、多次的審查,諮詢會議應該就只是審查行政流程有無問題,不會再被問什麼問題了。結果,沒想到在這個階段,還是會被問問題,而且是前面審查員都沒問過的大問題。麻煩的是,諮詢會議是有會期的,錯過了一個會期,就要慢~慢~等~下~去。
補件通知可能只有一句話、幾個字,看不懂那些專家為什麼要問這個問題?沒辦法,我們只能猜!因為在這個階段,一樣「不能」和諮詢會議的專家討論、說明,完全不能了解會議上的專家提出問題的原因,只能輾轉從食藥署承辦人那邊得知「大概」的問題,要我們靠著算命功力去回覆。
而且,諮詢會議上的專家看的文件,可能會是最初送進食藥署的版本,而不是中間多次補件、修改並遞交給 TAF 最新版本哦。
完全不懂為什麼前面那麼多人審查了,還換人審查,結果到最後一關,還會再被問先前流程中完全沒被問過的問題?也不能理解不讓我們和「專家」溝通,只透過承辦人轉達 + 含糊不清的公文,這要我們怎麼有效率地回覆?更不懂,怎麼會讓諮詢會議上的專家看的是舊版過期文件呢?
而我最大的不解是,怎麼搞得比醫療器材還麻煩哩?!是輸人不輸陣,我 LDTs 開發流程鬆散(根本沒有所謂的 Design Control 啦)、不用足夠的臨床證據,但是我審查流程可是比醫療器材嚴謹?
不過,我真的很謝謝食藥署的承辦人,我可以明顯感覺到他們很努力在幫忙我們這些業者,或許承辦人們也有點無奈(?)相較於醫事司,食藥署真是天使機構 ε٩(๑> ₃ <)۶з

實驗室認證流程可簡化成:提出申請 ➡ 形式審查 ➡ 書面審查 ➡ 實地查核 ➡ 專家綜合評估 ➡ 專家諮詢會議 ➡ 結案函。「形式審查」和「書面審查」兩階段的補件期限都只有 14 天,而「實地查核」後的補件期限有 60 天。
圖片來源:《精準醫療分子檢測實驗室認證相關注意事項》
關於第二階段流程 – 醫事司的「實驗室開發檢測施行計畫」,請見醫事司「申請實驗室開發檢測之相關須知事項」的《醫療機構施行實驗室開發檢測項目申請須知》。
另外,此階段的「醫療機構施行實驗室開發檢測項目申請計畫書」內看似需附上「醫檢師執業執照影本」,但詢問醫策會後說不用,在核准第一案後才會被要求去申請執業登記,理由是:「你們的申請計畫還沒被核准前,醫檢師也不能執業登記在你們實驗室下面。」
但是,衛部醫字第 1121664135 號(Backup)公告:「依《特定醫療技術檢查檢驗醫療儀器施行或使用管理辦法》第三十七條規定,經中央主管機關認證或取得經中央主管機關公告相關認證資格之實驗室,為《醫事檢驗師法》第九條所定其他經主管機關認可必須聘請醫事檢驗師之機構。」
依上面那份公告,只要取得食藥署的 LDTs 檢測實驗室認證,就可以讓醫檢師登記執業登記了吧?為什麼醫策會的人會說,「第一案計畫還沒被核准前,醫檢師無法執業登記在你們實驗室。所以,在醫療機構施行實驗室開發檢測第一案『後』,才需要繳交醫檢師執業登記」呢?
另外,各位如果時間有限,可能就不用浪費時間去詢問醫事司了。他們的老鳥從來不接電話、亂回函詢,同事幫忙留言給她也不回,散發著極度濃烈的擺爛氣息,似乎就是「你能拿我怎樣」的感覺(雖然我沒看到啦),而菜鳥就只會一直重複《特管辦法》的規定,也不敢去和老鳥確認。
我可以想像他們很忙,但 LDTs 是他們自己搞出來的。要搞,就好好搞,不要隨便做個表單交差了事,要公布表單前,可不可以先找內部幾個完全沒參與的人去試填看看,測試看不看得懂。做不好也沒關係,但要改啊!至少醫事司內部人員自己要清楚要繳交哪些資料吧!一直要求業界要教育訓練、要上課、要被稽核、要被審查,結果醫事司 LDTs 的人自己沒上課、沒考核?
後來,發現在 2024/09/06 的 《醫療機構施行實驗室開發檢測項目-申請及審查流程說明》第 39、40、42 頁分別有一小條註解:「國內認證實驗室之品質主管可暫不檢附執業執照,待相關法規通過後再行補件」、「國內認證實驗室之專任技術人員可暫不檢附執業執照,待相關法規通過後再行補件」、「如核發檢測報告之醫檢師任職於認證實驗室,可暫不檢附執業執照,待相關法規通過後再行補件」。
就這樣,一小條註解,不是由官方單位發公文,沒放在醫事司網站,也沒註解在施行計畫的申請表單中,僅僅在某個說明會的投影片中小小註解一下,甚至打電話去問醫事司的人也不知道要不要放執業執照,卻讓認真準備資料的人苦惱很久。
如果業者也是這樣做事,可以嗎?這麼任性且亂七八糟的做事方式,為何有資格可以要求業者好好做事呢 (┛`д´)┛
5.2 預計時程
提供我們自己「食藥署 LDTs 實驗室認證(第一階段)」實際時程供大家參考:
| 事件 | 距上一事件過了幾天? | 距「開始建立 QMS」 過了幾天? | 距「正式送件至 TFDA」過了幾天? |
|---|---|---|---|
| 開始建立 QMS | N/A | N/A | N/A |
| 正式送件至 TFDA | 181 | 181 | 0 |
| 收到形式審查補件公文 | 22 | 203 | 22 |
| 正式補件(形式審查) | 13 | 216 | 35 |
| 收到書面審查補件通知(第一次) | 44 | 260 | 79 |
| 正式補件 (第一次書面審查) | 15 | 275 | 94 |
| 收到書面審查補件通知(第二次) | 20 | 295 | 114 |
| 正式補件 (第二次書面審查) | 7 | 302 | 121 |
| 正式實地查核 | 8 | 310 | 129 |
| 收到實地查核缺失改善補件通知(第一次) | 7 | 317 | 136 |
| 回覆實地查核缺失改善結果(第一次) | 17 | 334 | 153 |
| 收到實地查核缺失改善補件通知(第二次) | 4 | 338 | 157 |
| 收到專家綜合評估(預行審議)補件通知 | 24 | 362 | 181 |
| 正式補件(專家綜合評估) | 2 | 364 | 183 |
| 收到專家諮詢會議補件通知(第一次) | 34 | 398 | 217 |
| 正式補件(第一次專家諮詢會議) | 1 | 399 | 218 |
| 收到專家諮詢會議補件通知(第二次) | 35 | 434 | 253 |
| 正式補件(第二次專家諮詢會議) | 2 | 436 | 255 |
| 正式核准 ( ´Д`)y━・~~ | 33 | 469 | 288 |
整個實驗室認證過程分成以下兩個大階段:
第一階段:建立 QMS
經過 181 天的準備後,品質系統終於堪用,也做完分析確效、Proficiency Testing(PT),正式送件至食藥署 TFDA。
第二階段:正式送件至 TFDA
我們從「建立 QMS」開始,過了 181 天才正式送件至食藥署 (TFDA);從「正式送件至 TFDA (Day 0)」到「正式核准」,又過了 288 天。
各位可以從上面注意到很多階段都會要求兩次補件,我覺得不是因為我們補不好,而是很多流程中,我們只能看著資訊非常不足的補件通知來推測(偉大的)委員專家們是為什麼問這個問題,沒法直接和他們溝通。甚至,我們還接過「只有一句話」共 20 個字的要求補充說明的公文。這簡直是單方面把補件公文當作 Line 來傳訊息嘛(飛鴿傳書的比喻比較貼切,因為很~~慢)!
另外,「書面審查」、「實地查核」、「專家綜合評估(預行審議)」、「專家諮詢會議」很可能(或是流程設計就是要)由不同的人審查,是有必要搞得「那麼嚴謹」哦?前面都已經被(偉大的)委員專家們查過了,後面又給不同的委員專家們審查,這樣後面的委員專家們如果不提意見,好像白收錢,提了意見,又好像打臉前面的委員專家們。
再來,因為至少是兩個機構,TFDA 和 TAF,合力完成整個流程,可能導致最後階段的委員專家們看到的文件版本不一定是改版後的版本。
總之,從「正式送件至食藥署」到「正式核准」,這 288 天心很累欸。(≖_≖)✧ 小孩都生出來了

冏rz… 不過,我目前遇到的都是好人啦,只是心有點累。
6. 認證核准後注意事項
每三年要展延一次,所以在到期日前的六到八個月就要向食藥署申請。並且,有可能會有無預警稽核,所以還是不能鬆懈。
當然,還是要注意後面會提到的變更管制,某些變更要在變更前,或變更後向食藥署申請,不是想變就變的喔!
不過,最不可思議的規定是:「必須於每年 3 月 1 日前檢送前一年度實撿室間比對方案或替代性評估相關資料至食藥署。」
依據《醫療器材安全監視管理辦法》第六、七條,以及《醫療器材上市後監督規範》,只有特定的醫療器材許可證所有人或登錄者,才需要定期繳交定期安全性報告至中央主管機關指定之網路系統。而且,是有「監視期間」的:「當於監視期間屆滿後 60 個日曆天內,須完成登載安全性總結報告。」之後,就不用繼續交報告了。
上述這個規定,也只有部分高風險醫材,經公告為「應執行安全監視之醫療器材品項」後,才需要定期繳交定期安全性報告。
LDTs 比這些高風險醫材還高風險,需要「永久」定期繳交報告給食藥署?如果是的話,那為何又說相較於 IVD,LDTs 可保有技術彈性?怎麼可以給 LDTs 這些彈性呢?
又或者,《精準醫療分子檢測實驗室檢測與服務指引符合性查核基準》缺少上市後的規範,所以才會訂定此項規定?如果是這樣,那就新增這些規定呀!反正《LDTs 查核基準》本來也就不是百分之百照 ISO 15189:2012 了嘛。
7. 其他注意事項
7.1 不可直接與受檢者接觸
在《特管辦法》所規定的 LDTs 管理架構中,特定實驗室不可直接和病人直接接觸,須由醫療機構委託始可施行 LDTs,此項規定從 LDTs 管理架構中可以看出來。這個架構會影響到一些實驗室內的文件內容、表格設計、流程規劃。例如:實驗室從醫療機構接收到的資料中,(照理說)不可以有「受檢者的姓名、身分證字號等足以辨識個人之資料」(請見《精準醫療分子檢測實驗室檢測與服務指引符合性查核基準》「5.1.6 樣本接收」)。
醫事司司長劉越萍在 2024 年 12 月由台灣精準醫療產業協會(PMIA Taiwan)主辦的「LDTs 特管辦法與健保給付專家座談會」上說:「因為管理 LDTs 的《特管辦法》是依《醫療法》所制訂的,所以是由醫療機構與受試者接觸,不可直接由檢測實驗室去接觸。」
但我就覺得奇怪,那為什麼要選《醫療法》呢?為什麼不選《藥事法》甚至《醫療器材管理法》呢?明明依照《醫療器材管理法》第 3 條對於「醫療器材」的定義,LDTs 就是醫療器材嘛!要嘛就像美國那樣有種,把 LDTs 定義為:LDTs are in vitro diagnostic products (IVDs) that are intended for clinical use and are designed, manufactured, and used within a single laboratory.(LDTs(實驗室自行開發檢測)是體外診斷產品(IVDs),其目的是用於臨床用途,並於單一實驗室內設計、製造及使用。)
另外,我又想要繼續抱怨!
為何相較於 IVD,LDTs 可以保有「技術彈性、技術多樣項、價格有競爭力」等特性呢?(Ref:顧文輝與張偉嶠觀點:LDTs 與 IVD 將共存共融)我覺得就是因為 LDTs 的監管法規寬鬆。為什麼 LDTs 監管法規可以比較寬鬆呢?因為 LDTs 風險等級比 IVD 低。但現在《特管辦法》一搞,食藥署、醫事司審一堆東西,搞得好像沒有比較有彈性,流程也非常繁瑣不透明。要不乾脆就併入《醫療器材管理法》,劃出一個第零等級給 LDTs 嘛 (`へ´≠)
7.2 儘早確認實驗室間比對方案
精準醫療分子檢測實驗室施行實驗室開發檢測(Laboratory Developed Tests,LDTs),為確保檢驗流程及報告產出之品質,實驗室需定期參與外部能力試驗執行機構辦理的能力試驗活動,作為實驗室確認量測結果正確性的監控活動之一;當無能力試驗活動可參加時,實驗室得邀約其他同儕實驗室辦理實驗室間比對活動,透過實驗室間能力比對,評估實驗室品質、測試及報告產出的能力,確保服務對象得到可信賴與精確之檢測結果。
– 《精準醫療分子檢測實驗室間比對與替代性評估指引》
因此,如果所提供的 LDTs 可以找到適合的外部專業機構舉辦的能力試驗(Proficiency Testing,PT),那就必須提早準備,避免特定 PT 一年只舉行一次,錯過了,還要再等一年。
關於這部分,在《精準醫療分子檢測實驗室檢測與服務指引符合性查核基準》「5.3.3 實驗室間比對」有詳細的介紹。
7.3 LDTs 只可和醫療機構合作施行
7.3.1 錯誤認知
過去,我(公司)認為只要不是在醫療機構執行 LDTs,那就不用管《特管辦法》,當然也不用遵循依著《特管辦法》所制訂出的《精準醫療分子檢測實驗室檢測與服務指引符合性查核基準》建立特定實驗室,更不用申請第二階段醫事司的「實驗室開發檢測施行計畫」。
首先,電話詢問了醫策會:
《特管辦法》只管醫療機構,我們也只依《特管辦法》做事。」不知名的承辦人如是說。
我解讀的醫策會承辦人的言下之意就是:「你要跟非醫療機構做 LDTs 的話,我管不著啦!」
接著,我收到了醫事司的回覆:
《醫師法》第 28 條所稱「醫療業務」行為,係指以治療、矯正或預防人體疾病、傷害、殘缺為目的,所為之診察、診斷及治療;或基於診察、診斷結果以治療為目的,所為處方、用藥、施術或處置等行為全部或一部的總稱,合先敘明。依上揭規定,貴公司開發之癌症檢測技術,若以疾病診斷為目的,係屬醫療業務,應由醫師親自為之或相關醫事人員依其各該專門執業法律所規定之業務依醫囑行之。
我解讀的醫事司言下之意就是:「只要你找得到『醫師,或者相關醫事人員依其各該專門執業法律所規定之業務及醫囑』,就可以做 LDTs 啦,不用管是不是在醫療機構!」所以,我只要在非醫療機構找到醫師願意合作 LDTs,那就不用經歷漫漫長路的兩階段申請了。(為什麼醫事司不正答我的問題呢?繞來繞去,結果還是沒有明確、直接、正面回答我的問題:「若 LDTs 在「非醫療機構」執行,是否仍需提交施行計畫及申請核准,還是可直接執行?」(┛`д´)┛)
另外,我自己研究了一下:
在醫事司網頁「申請實驗室開發檢測之相關須知事項」中有明確指出:「依據《特管辦法》第 7 條及第 36 條規定,醫療機構施行實驗室開發檢測,應擬定施行計畫,向本部申請並經核准後,始得為之。」
同時,依據「衛部醫字第 1101668673 號」公告,衛福部依《特管辦法》第 37 條第 6 項委託食藥署執行 LDTs 實驗室認證相關事項。
無論食藥署或醫事司,都是因《特管辦法》而有職權進行兩階段的認證。看了《特管辦法》第 7、36 及 37 條規定,都僅適用於「醫療機構」執行 LDTs,沒有管到非醫療機構,並且《特管辦法》也沒說 LDTs 「只」可在醫療機構執行。
因此「感覺上」《特管辦法》僅規範「醫療機構內」施行 LDTs,不包括「非醫療機構」,所以證成當時的錯誤認知:只有在醫療機構施行 LDTs 前需要(1)申請食藥署的「精準醫療分子檢測實驗室認證」,以及(2)向醫事司的「醫療機構施行實驗室開發檢測項目申請計畫」。
另外還有下兩點:
(1)醫事司的「醫療機構施行實驗室開發檢測項目申請計畫」,從計畫名稱看起來就只管「醫療機構」,不然,應該改為「施行實驗室開發檢測項目申請計畫」不需要多寫「醫療機構」嘛!
(2)整篇《特管辦法》全部都在說:「『醫療機構』施行非人體試驗之細胞治療技術、『醫療機構』施行第二十五條所定特定美容醫學手術項目、『醫療機構』施行第二章第三節所定其他特定醫療技術項目、『醫療機構』施行或使用第三章第一節所定特定醫療儀器項目、『醫療機構』施行第三章第二節所定特定檢查、檢驗之實驗室開發檢測項目…」看起來全都是「在醫療機構內」執行才列管。
如果 LDTs 只可在醫療機構做,那至少應該刪去《特管辦法》第 37 條第 1 項的「醫療機構」,改成「施行實驗室開發檢測,應由經中央主管機關認證,或取得經中央主管機關公告相關認證資格之實驗室或醫事檢驗所(以下併稱認證實驗室)為之。」
7.3.2 疑惑的點
可是,真的是在非醫療機構做 LDTs 就啥都不用管(用自來水在廚房做 LDTs 都可以)嗎?但是《特管辦法》第 37 條第 5 項規定,施行 LDTs 的實驗室設於境外者要向中央主管機關申請許可,怎麼反而會讓境內非醫療機構做 LDTs 可以不用被列管呢?
7.3.3 正確解答
但在詢問了食藥署後,情勢大轉。食藥署明確表示「LDTs 只可和醫療機構合作施行」。以下是食藥署的回覆:
《特定醫療技術檢查檢驗醫療儀器施行或使用管理辦法》(下稱特管法)係依《醫療法》第 62 條第 2 項規定訂定,故 LDTs 屬《特管法》規範之特殊檢驗範疇,又《特管法》第 7 條規定「醫療機構」施行 LDTs,應檢具相關文件、資料(含同法第 36 條所定施行計畫),向中央主管機關申請核准後,經直轄市、縣(市)主管機關登記,始得為之。是以,該法並未授權「非」醫療機構可申請施行計畫,且未依前述規定取得衛福部醫事司核准,特定實驗室亦不得施行 LDTs。
並且,食藥署承辦人也和我說,在與醫事司溝通確認過後,兩個單位一致都認為:「LDTs 只可和醫療機構合作施行」。
(不過,食藥署提到的《醫師法》第 8-2 條規定醫師可以在「核准登記之醫療機構、長期照顧服務機構、精神復健機構或其他經中央主管機關認可之機構」內執業,似乎並沒有規定只能在醫療機構內執業;《醫療法》第 62 條第 2 項只有授權中央主管機關可訂定辦法去管理特定醫療技術、檢查、檢驗或醫療儀器,並沒有規範管理細節;《特管辦法》第 7 條也只規定,若 LDTs 在醫療機構施行時,必須遵守規定,但沒說 LDTs 「只」可以在醫療機構內施行,或與醫療機構合作施行。
所以,無論從《醫師法》、《醫療法》或《特管辦法》,還是都看不出哪裡有規定醫療業務、醫療行為「只能」在醫療機構內執行。)(但還是非常感謝食藥署啦 (*‘ v`*),比醫事司好溝通多了!)
對於結果,雖然還是疑惑,但也只能接受。冏rz…
7.4 違規的罰則是什麼?
根據《特定醫療技術檢查檢驗醫療儀器施行或使用管理辦法》第 37 條規定,醫療機構若要進行實驗室開發檢測(Laboratory Developed Tests,LDTs),必須由經認證的實驗室執行。
此外,該辦法第 39 條規定,認證實驗室應 (1) 依據醫師開立的醫囑,並 (2) 按照其通過認證的檢測項目提供服務。
若認證實驗室有以下情形之一,中央主管機關可依第 42 條規定,停止或終止其部分或全部的實驗室開發檢測項目:
- 未依認證之檢測項目提供服務。
- 無醫囑或未依醫囑施行檢測。
- 未依第 39 條規定製作紀錄、出具報告,或簽名、蓋章。
- 製作不實紀錄,或出具不實報告。
- 違反第 37 條第 3 項規定,未取得中央主管機關認證或變更許可。
- 違反第 37 條第 4 項規定,規避、妨礙或拒絕中央主管機關查核。
- 未依第 40 條第 1項或第 2 項規定,提供紀錄或報告予醫療機構;或提供、洩露予委託之醫療機構以外之第三人。
- 違反其他法規嚴重影響受檢者權益、安全之情事。

8. LDTs 查核基準
食藥署的《精準醫療分子檢測實驗室檢測與服務指引符合性查核基準》是依據舊版 ISO 15189:2012 翻譯、微調而成的,是申請「精準醫療分子檢測實驗室認證」最重要依據,業界實驗室要依據《查核基準》建立實驗室品質管理系統(QMS),並通過稽核成為特定實驗室。
以下,就來分享一下怎樣實現《查核基準》的規定吧。

又想抱怨一下!這個《查核基準》的內容、格式、排版真是不容易看。
明明就是用 ISO15189:2012,但台灣政府總愛自己調整一下。調整就算了,翻譯品質也不是很好,語句不順很常見,並且有些在 ISO15189:2012 中不同段落的同樣英文單字,卻在《查核基準》中沒有統一的中文翻譯。甚至,還會看到似乎是沒寫完的句子!
除了翻譯問題外,還有槓掉的內容。如果說是想要讓我們業者可以了解《查核基準》和 ISO15189:2012 原文的差異而保留中文翻譯並加以槓掉,那很棒。但有些地方《查核基準》卻不是選擇保留中文翻譯+槓掉,而是直接消失。
最後,《查核基準》甚至還有出現某些內容有劃底線?劃底線是想要表達這很重要?那其他沒劃底線的內容比較不重要?還是,這只是某員工的個人筆記?
哦~還有,《查核基準》的 8.6 檢測項目確效與驗證說是和 ISO15189:2012 的 5.1.9 章節相關。不過,ISO15189:2012 的 5.1.9 章節是「Personnel records」,和「檢測項目確效與驗證」似乎不相關。
不用說這份《查核基準》的 PDF 還有莫名的空格、無法正常從 PDF 複製下來、不知道是排版還是缺漏字導致語意不明確等問題了。
《查核基準》是國家級大機構所發行的規定,要求全中華民國相關業者都要遵循,正常來說,應該是用極為嚴謹的態度,再三審查、檢視,確認沒問題後再公布吧 ( ˘•ω•˘ )
8.1 人員及設備要求
人員資格
實驗室應明定所有人員的職責、權責及工作任務,實驗室人員須具相當之知識背景。
| LDTs 查核基準 | ISO 15189:2012,5.1.1 – 5.1.4 |
|---|---|
| 1.1 人員資格 1.1.1 概述 – 實驗室應有人員管理的文件化程序與維持所有人員的紀錄,以顯示符合要求。 1.1.2 人員資格 – 實驗室管理階層應針對每個職位之人員資格予以文件化。此資格應能呈現其適當的教育、訓練、經驗及所需的技能證明,並適任所執行的工作任務。涉及檢測判斷的人員,應具備適用的理論與實務背景及經驗。 附註:專業判斷能以意見、解釋、預測、模擬與模式及數值等表示,並須符合國家、區域及地方法規及專業指引。 1.1.3 工作說明 – 實驗室應有工作說明,以說明所有人員的職責、權責及工作任務。 1.1.4 人員之組織環境介紹 – 實驗室應有一套方案,向新進員工介紹組織、其將就任的部門或區域、受雇的契約與條件、員工設施、健康與安全要求(包括火警與緊急狀況)及職業健康服務等。 | 5.1.1 General The laboratory shall have a documented procedure for personnel management and maintain records for all personnel to indicate compliance with requirements. 5.1.2 Personnel qualifications Laboratory management shall document personnel qualifications for each position. The qualifications shall reflect the appropriate education, training, experience and demonstrated skills needed, and be appropriate to the tasks performed. The personnel making judgments with reference to examinations shall have the applicable theoretical and practical background and experience. NOTE Professional judgements can be expressed as opinions, interpretations, predictions, simulations and models and values, and should be in accordance with national, regional and local regulations and professional guidelines. 5.1.3 Job descriptions The laboratory shall have job descriptions that describe responsibilities, authorities and tasks for all personnel. 5.1.4 Personnel introduction to the organizational environment The laboratory shall have a programme to introduce new staff to the organization, the department or area in which the person will work, the terms and conditions of employment, staff facilities, health and safety requirements(including fire and emergency), and occupational health services. |
建議符合方式:
《教育訓練與員工資格管理程序》中明訂「每個職位之人員資格」與「如何向新進員工工作、部門、公司相關事務」;《組織權責與代理人程序》則制訂「所有人員的職責、權責及工作任務」。
最重要的還是「要有醫檢師」呀!(這是《特管辦法》的重點呀 ㄟ( ▔, ▔ )ㄏ)
能力評鑑
實驗室應定期考評每位人員執行受指派管理或受指派技術任務之能力。
| LDTs 查核基準 | ISO 15189:2012,5.1.6 – 5.1.7 |
|---|---|
| 1.2 能力評鑑 1.2.1 能力評鑑 – 在適當的訓練後,實驗室應依據所建立之準則,評鑑每位人員於執行受指派的管理或技術任務之能力。 – 再評鑑應定期實施。當必要時,應辦理再訓練。 附註 1:與一般工作環境相同條件下,可使用下列任何組合或所有方式, 評鑑實驗室人員的能力: a)直接觀察例行工作流程與程序,包括所有適用的安全操作; b)直接觀察設備維護與功能檢查; c)監控其記錄與發放檢測結果; d)工作紀錄的審查; e)問題解決技能的評鑑; f)提供特殊樣本執行檢測,如先前已完成檢測的樣本、實驗室間比對材料或分割樣本。 附註 2:專業判斷的人員能力評鑑,須經特別設計並符合其目的。 | 5.1.6 Competence assessment Following appropriate training, the laboratory shall assess the competence of each person to perform assigned managerial or technical tasks according to established criteria. Reassessment shall take place at regular intervals. Retraining shall occur when necessary. NOTE 1 Competence of laboratory staff can be assessed by using any combination or all of the following approaches under the same conditions as the general working environment: a)direct observation of routine work processes and procedures, including all applicable safety practices; b)direct observation of equipment maintenance and function checks; c)monitoring the recording and reporting of examination results; d)review of work records; e)assessment of problem solving skills; f)examination of specially provided samples, such as previously examined samples, interlaboratory comparison materials, or split samples. NOTE 2 Competency assessment for professional judgment should be designed as specific and fit for purpose. 5.1.7 Reviews of staff performance In addition to the assessment of technical competence, the laboratory shall ensure that reviews of staff performance consider the needs of the laboratory and of the individual in order to maintain or improve the quality of service given to the users and encourage productive working relationships. NOTE Staff performing reviews should receive appropriate training. |
建議符合方式:
在《教育訓練與員工資格管理程序》中明訂,執行工作前要依此本程序書受訓並考核。
要注意的是,「再評鑑」必須定期實施,例如,每年第四季評估,不是只有新進人員評鑑完就沒事了(not just a one-and-done event)。若再評鑑老員工時發現問題,還需要再訓練,之後再評鑑。
另外還要注意《特管辦法》第 38 條的特殊規定,要記得上完「實驗室開發檢測之實驗室人員訓練課程」,並且必須取得證書。
可以把這些規定都寫到《教育訓練與員工資格管理程序》避免忘記。
教育訓練
實驗室人員需要接受持續教育訓練。
| LDTs 查核基準 | ISO 15189:2012,5.1.8 |
|---|---|
| 1.3.1 持續教育與專業發展 – 應提供參與管理與技術流程的人員的持續教育方案。人員應參與持續教育。持續教育方案之有效性應定期加以審查。 – 人員應定期參與專業發展或其他專業交流活動。 | 5.1.8 Continuing education and professional development A continuing education programme shall be available to personnel who participate in managerial and technical processes. Personnel shall take part in continuing education. The effectiveness of the continuing educationprogramme shall be periodically reviewed. Personnel shall take part in regular professional development or other professional liaison activities. |
建議符合方式:
在《教育訓練與員工資格管理程序》中規劃參與管理與技術流程的人員的持續教育方案。可以每年第四季創建一個明年度的「年度教育訓練計畫」,讓各單位去受(內 / 外)訓。
人力資源紀錄
實驗室應保存所有與人員相關學歷、專業資格、教育訓練、經驗及能力考評相關紀錄。
| LDTs 查核基準 | ISO 15189:2012,5.1.9 |
|---|---|
| 1.4.1 人員紀錄 – 所有與人員相關教育與專業資格、訓練與經驗、及能力評鑑的相關紀錄,應加以維持。這些紀錄應可供相關人員方便取得,且應包括但不限於以下: a)教育與專業資格; b)證書或執照的影本,當適用時; c)先前的工作經驗; d)工作說明; e)新進人員之實驗室環境介紹; f)目前工作任務的訓練; g)能力評鑑; h)持續教育與個人成就的紀錄; i)員工服務表現的審查; j)意外事故與曝露於職業危害的報告; k)與指派職務相關的疫苗接種狀況。 附註:上述所列紀錄不要求儲存於實驗室,但可維持於其他特定地點,當需要時,可隨時取得。 | 5.1.9 Personnel records Records of the relevant educational and professional qualifications, training and experience, and assessments of competence of all personnel shall be maintained. These records shall be readily available to relevant personnel and shall include but not be limited to: a)educational and professional qualifications; b)copy of certification or license, when applicable; c)previous work experience; d)job descriptions; e)introduction of new staff to the laboratory environment; f)training in current job tasks; g)competency assessments; h)records of continuing education and achievements; i)reviews of staff performance; j)reports of accidents and exposure to occupational hazards; k)immunisation status, when relevant to assigned duties. NOTE The records listed above are not required to be stored in the laboratory, but can be maintained in other specified locations, providing they remain accessible as needed. |
建議符合方式:
除了在《教育訓練與員工資格管理程序》中規定各個不同角色、職位的新進人員要繳交並確認哪些資格、文件(例如,學歷證書、醫檢師執照),要被教導哪些知識、資訊(例如,工作說明、實驗室環境介紹)之外,還可以創建《文件與紀錄管理程序》用來管理各類文件,以及這邊提到的教育訓練、資格相關的紀錄。
設施與環境條件
實驗室為執行其工作,應有適當空間設計,以確保提供品質、安全性及有效性的服務給使用者,並確保其安全。
| LDTs 查核基準 | ISO 15189:2012,5.2 |
|---|---|
| 1.5 設施與環境條件 1.5.1 概述 – 實驗室為執行其工作,應有空間分配的設計,以確保提供品質、安全性及有效性的服務予使用者,並確保實驗室人員、訪客的健康與安全。 – 為執行其工作,實驗室應評估與決定空間分配的足夠性與適當性。 1.5.2 實驗室與辦公室設施 – 實驗室與相關的辦公室設施,應提供適合執行工作任務的環境,並劃分感染性和非感染性區域,以確保符合下列情況: a)對於影響檢測品質區域的進出加以管制。 附註:進出管制須考量安全、機密、品質及實務操作。 b)醫療資訊、樣本及實驗室資源加以安全防護,避免未經授權取得。 c)檢測設施有考量到檢測的正確執行。這些包括,舉例如能源、照明、通風、噪音、用 水、廢棄物處理與環境條件等。 d)實驗室內部通訊系統能適用於設施的規模與複雜性,以確保資訊的有效傳輸。 e)提供安全設施與裝置,並定期查證其功能。 舉例:冷房(cold rooms)與進出式冷藏室(walk-in freezers)的緊急逃生裝置、內部對講機與及警報系統;緊急淋浴與洗眼器的可取得等。 1.5.3 儲存設施 – 應提供相關儲存空間與條件,以確保樣本物質、文件、設備、試劑、耗材、紀錄、結果、及任何可影響檢測結果品質的其他項目之完整性。 – 用於檢測流程的檢體與物質應予以妥善儲存,以避免交互污染。 – 危險物質儲存與棄置的設施,應適用於物質的危害性與其特定適用要求。 1.5.4 員工設施 – 應可取用充足的洗手間、飲用水的供應,以及個人防護性設備儲存與更衣的設施。 附註:當可能時,實驗室須提供員工活動空間,例如會議室、研究與休憩的安靜區域。 1.5.6 設施維持與環境條件 – 實驗室場所應維持功能性與可靠的條件。工作區應予清潔且維持良好。 – 當相關規格有所要求,或它們對樣本、結果的品質與或員工健康會影響時,實驗室應監控、管制及記錄環境條件。 – 應注意下列因素,如照明、消毒、灰塵、毒氣或危害性氣體,電磁干擾、輻射、濕度、電源供應、溫度、聲音與震動程度及工作流程物流等,以適於所考量作業活動,因此這些因素不會使結果無效或對檢測品質有不良影響。 – 不相容活動的實驗室區域應有效地隔離。 – 當檢測程序暴露危害或工作因未隔離而可能被感染或影響時,應採取程序以預防交互污染。 – 當需求時,實驗室應提供一個安靜且不被打擾的工作環境。 附註:安靜且不受打擾的工作區域,舉例包括細胞病理學的篩檢,血球細胞與微生物的鏡檢分類、定序反應的數據分析以及分子突變結果的審查。 | 5.2 Accommodation and environmental conditions 5.2.1 General The laboratory shall have space allocated for the performance of its work that is designed to ensure the quality, safety and efficacy of the service provided to the users and the health and safety of laboratory personnel, patients and visitors. The laboratory shall evaluate and determine the sufficiency and adequacy of the space allocated for the performance of the work. 5.2.2 Laboratory and office facilities The laboratory and associated office facilities shall provide an environment suitable for the tasks to be undertaken, to ensure the following conditions are met. a)Access to areas affecting the quality of examinations is controlled. NOTE Access control should take into consideration safety, confidentiality, quality and prevailing practices. b)Medical information, patient samples, and laboratory resources are safeguarded from unauthorized access. c)Facilities for examination allow for correct performance of examinations. These include, for example, energy sources, lighting, ventilation, noise, water, waste disposal and environmental conditions. d) Communication systems within the laboratory are appropriate to the size and complexity of the facility to ensure the efficient transfer of information. e) Safety facilities and devices are provided and their functioning regularly verified. EXAMPLE Operation of emergency release, intercom and alarm systems for cold rooms and walk-in freezers; accessibility of emergency showers and eyewash, etc. 5.2.3 Storage facilities Storage space and conditions shall be provided that ensure the continuing integrity of sample materials, documents, equipment, reagents, consumables, records, results and any other items that could affect the quality of examination results. Clinical samples and materials used in examination processes shall be stored in a manner to prevent cross contamination. Storage and disposal facilities for dangerous materials shall be appropriate to the hazards of the materials and as specified by applicable requirements. 5.2.4 Staff facilities There shall be adequate access to washrooms, to a supply of drinking water and to facilities for storage of personal protective equipment and clothing. NOTE When possible, the laboratory should provide space for staff activities such as meetings and quiet study and a rest area. NOTE Some facilities may need equipment appropriate for resuscitation; local regulations may apply. 5.2.6 Facility maintenance and environmental conditions Laboratory premises shall be maintained in a functional and reliable condition. Work areas shall be clean and well maintained. The laboratory shall monitor, control and record environmental conditions, as required by relevant specifications or where they may influence the quality of the sample, results, and/or the health of staff. Attention shall be paid to factors such as light, sterility, dust, noxious or hazardous fumes, electromagnetic interference, radiation, humidity, electrical supply, temperature, sound and vibration levels and workflow logistics, as appropriate to the activities concerned so that these do not invalidate the results or adversely affect the required quality of any examination. There shall be effective separation between laboratory sections in which there are incompatible activities. Procedures shall be in place to prevent cross-contamination where examination procedures pose a hazard or where work could be affected or influenced by not being separated. The laboratory shall provide a quiet and uninterrupted work environment where it is needed. NOTE Examples of a quiet and uninterrupted work area include cytopathology screening, microscopic differentiation of blood cells and microorganisms, data analysis from sequencing reactions and review of molecular mutations results. |
建議符合方式:
《設施與環境維護程序》可用來規劃及規定實驗室環境、管理基礎設施,《設備軟體與資訊系統維護程序》則負責規範基礎設施所使用的軟體以及資訊管理系統。
《查核基準》刪除了 ISO 15189:2012 的 5.2.5 章節(Patient sample collection facilities),因為在 LDTs 的管理架構下,一般業界的實驗室不能與受試者接觸,所以也不會有檢體採檢設施。
實驗室設備
實驗室對其設備及試劑之選擇、採購及管理應有文件化要求,並執行相關品質管理政策以確保其品質。
| LDTs 查核基準 | ISO 15189:2012,5.3 |
|---|---|
| 1.6 實驗室設備、試劑及耗材 附註 1:為了符合此國際標準,實驗室設備包括儀器的硬體與軟體、量測系統及實驗室資訊系統。 附註 2:試劑包括參考物質、校正物質與品管物質;耗材包括培養基、微量吸管的尖管(tips)、玻片等。 附註 3:選擇與採購外部服務、設備、試劑及耗材等資訊考量,請參考 4.3。 1.6.1 設備 1.6.1.1 概述 – 實驗室應有文件化的程序,作為設備的選擇、採購及管理。 – 實驗室提供服務業務所需之所有設備(包括樣本準備、樣本處理、檢測及儲存)應予以配置。 – 在某些情況下,當實驗室需使用非固有管制的設備時,實驗室管理階層應確保其設備滿足本規範的要求。 – 實驗室應依需求更新設備,以確保檢測結果的品質。 1.6.1.2 設備驗收測試 – 實驗室設備於安裝與使用前,應查證可達到所需性能並符合所考量的任何檢測相關要求(同時參見 5.2.1)。 附註:此要求適用於:實驗室內使用的設備、實驗室租賃的設備、在關聯或移動式設施由其他實驗室授權使用的設備。- 每項設備應給予唯一的標籤、標誌或不同識別。 1.6.1.3 設備使用說明- 任何時候,設備應由已訓練且授權人員操作。 – 製造商提供的設備使用、安全及維護保養的現行版本說明,包括任何相關的使用手冊與指導說明,應可隨時取閱。 – 實驗室應有程序以安全操作、運輸、儲存及使用設備,以防止污染或損壞。 1.6.1.4 設備校正與量測追溯 – 實驗室應有文件化的程序,作為直接或間接影響檢測結果設備的校正。此程序包括: a)考量使用的條件與製造商的說明; b)記錄校正標準的量測追溯與此設備的項目之可追溯校正; c)在明訂週期內,查證所要求的量測準確度與量測系統的功能; d)記錄校正狀況與再校正的日期; e)當由校正產生一組修正係數時,確保先前校正係數已正確更新; f)安全防護以防止因調整或竄改而使檢測結果無效。 – 量測追溯應追溯至可獲得的較高量測等級之參考物質或參考程序。 附註:對於較高等級參考物質或參考程序之校正追溯性的文件,可由檢測系統的製造商提供。只有使用未經過修正的製造商之檢測系統與校正程序,該份文件才可接受。 – 當其不可能或是無相關時,其他可提供結果信心的方式,應予適用,包括但不限於下列: .驗證參考物質的使用; .使用其它檢測或校正程序; .各相關團體已清楚確立、具體說明、特性清楚及相互承認的標準或方法。 1.6.1.5 設備維護保養與維修 – 實驗室應有一套文件化的預防維護保養方案,至少依循製造商的說明。 – 設備應維持在安全的工作條件與正常運作。其檢查應包括電器安全、緊急停止裝置(當具備時)、以及被授權的人員對化學、放射性與生物物質之安全處理與棄置。至少應使用製造商時程表或說明書(或兩者)。 – 不論何時,只要設備發現有缺點,應予停止服務與清楚地標示。實驗室應確保有缺點的設備未被使用,直到其經過維修且經查證顯示符合特定可接受準則為止。 – 實驗室應檢查任何缺點對先前檢測的影響,並開始執行立即措施或矯正措施(見 3.2)。 – 在服務、維修、或解除任務前,實驗室應採取適當的措施,以去除設備的污染與提供合適的維修空間與適當的個人防護設備。 – 當設備脫離實驗室的直接管制時,在回復使用前,實驗室應確保該設備性能已經查證。 1.6.1.6 設備不良事件通報 – 不良事件與意外事故可直接歸咎於特定設備時,應加以調查。當有要求時,通報製造商與適當權責機關。 1.6.1.7 設備紀錄 – 對檢測的性能有關的每項設備,應維持其紀錄。這些設備紀錄應包括,但不限於下列: a)設備的識別; b)製造商名稱、型號及序號或其他唯一識別; c)供應商或製造商的連絡資訊; d)接收的日期與加入服務的日期; e)位置; f)接收時的條件(例如,全新、使用過或整修過的); g)製造商的說明; h)設備納入實驗室時,證實設備於初始可接受使用的紀錄; i)已執行的維護保養與預防性維護保養時程; j)證實設備可持續接受使用的性能紀錄; k)設備損壞、或故障、修改或維修。 – 關於 j)項之性能紀錄,應包括所有校正與或查證報告 / 證書之副本,包括日期、時間與結果、調整、接受準則與下次校正及或查證到期日,以符合部份或全部本要求。 – 在設備使用期限,這些紀錄應加以維持並可供隨時取閱。或依實驗室紀錄管制程序的規定(見 3.4)保存更長期限。 | 5.3 Laboratory equipment, reagents, and consumables NOTE 1 For the purposes of this International Standard, laboratory equipment includes hardware and software of instruments, measuring systems, and laboratory information systems. NOTE 2 Reagents include reference materials, calibrators and quality control materials; consumables include culture media, pipette tips, glass slides, etc. NOTE 3 See 4.6 for information concerning the selection and purchasing of external services, equipment, reagents and consumables. 5.3.1 Equipment 5.3.1.1 GeneralThe laboratory shall have a documented procedure for the selection, purchasing and management of equipment. The laboratory shall be furnished with all equipment needed for the provision of services(including primary sample collection, sample preparation, sample processing, examination and storage). In those cases where the laboratory needs to use equipment outside its permanent control, laboratory management shall ensure that the requirements of this International Standard are met. The laboratory shall replace equipment as needed to ensure the quality of examination results. 5.3.1.2 Equipment acceptance testing The laboratory shall verify upon installation and before use that the equipment is capable of achieving the necessary performance and that it complies with requirements relevant to any examinations concerned(see also 5.5.1) NOTE This requirement applies to: equipment used in the laboratory, equipment on loan or equipment used in associated or mobile facilities by others authorized by the laboratory. Each item of equipment shall be uniquely labelled, marked or otherwise identified. 5.3.1.3 Equipment instructions for use Equipment shall be operated at all times by trained and authorized personnel. Current instructions on the use, safety and maintenance of equipment, including any relevant manuals and directions for use provided by the manufacturer of the equipment, shall be readily available. The laboratory shall have procedures for safe handling, transport, storage and use of equipment to prevent its contamination or deterioration. 5.3.1.4 Equipment calibration and metrological traceability The laboratory shall have a documented procedure for the calibration of equipment that directly or indirectly affects examination results. This procedure includes: a)taking into account conditions of use and the manufacturer’s instructions; b)recording the metrological traceability of the calibration standard and the traceable calibration of the item of equipment; c)verifying the required measurement accuracy and the functioning of the measuring system at defined intervals; d)recording the calibration status and date of recalibration; e)ensuring that, where calibration gives rise to a set of correction factors, the previous calibration factors are correctly updated; f)safeguards to prevent adjustments or tampering that might invalidate examination results. Metrological traceability shall be to a reference material or reference procedure of the higher metrological order available. NOTE Documentation of calibration traceability to a higher order reference material or reference procedure may be provided by an examination system manufacturer. Such documentation is acceptable as long as the manufacturer’s examination system and calibration procedures are used without modification. Where this is not possible or relevant, other means for providing confidence in the results shall be applied, including but not limited to the following: – use of certified reference materials; – examination or calibration by another procedure; – mutual consent standards or methods which are clearly established, specified, characterized and mutually agreed upon by all parties concerned. 5.3.1.5 Equipment maintenance and repair The laboratory shall have a documented programme of preventive maintenance which, at a minimum, follows the manufacturer’s instructions. Equipment shall be maintained in a safe working condition and in working order. This shall include examination of electrical safety, emergency stop devices where they exist and the safe handling and disposal of chemical, radioactive and biological materials by authorized persons. At a minimum, manufacturer’s schedules or instructions, or both, shall be used. Whenever equipment is found to be defective, it shall be taken out of service and clearly labelled. The laboratory shall ensure that defective equipment is not used until it has been repaired and shown by verification to meet specified acceptance criteria. The laboratory shall examine the effect of any defects on previous examinations and institute immediate action or corrective action(see 4.10). The laboratory shall take reasonable measures to decontaminate equipment before service, repair or decommissioning, provide suitable space for repairs and provide appropriate personal protective equipment. When equipment is removed from the direct control of the laboratory, the laboratory shall ensure that its performance is verified before being returned to laboratory use. 5.3.1.6 Equipment adverse incident reporting Adverse incidents and accidents that can be attributed directly to specific equipment shall be investigated and reported to the manufacturer and appropriate authorities, as required. 5.3.1.7 Equipment records Records shall be maintained for each item of equipment that contributes to the performance of examinations. These equipment records shall include, but not be limited to, the following: a)identity of the equipment; b)manufacturer’s name, model and serial number or other unique identification; c)contact information for the supplier or the manufacturer; d)date of receiving and date of entering into service; e)location; f)condition when received(e.g. new, used or reconditioned); g)manufacturer’s instructions; h)records that confirmed the equipment’s initial acceptability for use when equipment is incorporated in the laboratory; i)maintenance carried out and the schedule for preventive maintenance; j)equipment performance records that confirm the equipment’s ongoing acceptability for use; k)damage to, or malfunction, modification, or repair of the equipment. The performance records referred to in j) shall include copies of reports/certificates of all calibrations and/or verifications including dates, times and results, adjustments, the acceptance criteria and due date of the next calibration and/or verification, to fulfil part or all of this requirement. These records shall be maintained and shall be readily available for the lifespan of the equipment or longer, as specified in the laboratory’s Control of Records procedure(see 4.13). |
建議符合方式:
《供應商及採購管理程序》可用來評鑑供應商以及管理採購流程,並用《設備、試劑及耗材管理程序》管理設備(包含直接影響檢驗品質的量測與非量測儀器)、保養、定期校驗、標識、試劑與耗材的驗收,以及相關紀錄。當然,也可以用《文件與紀錄管理程序》來管理這邊所產生的紀錄。
另外,可以統一用《不符合事件管理程序》管理所有已發生或將發生的不正常狀況,利用補救、矯正及預防去防患未然或避免再次發生。
實驗室試劑及耗材
| LDTs 查核基準 | ISO 15189:2012,5.3 |
|---|---|
| 1.6.2 試劑與耗材 1.6.2.1 概述 – 實驗室應有文件化的程序,作為試劑與耗材之接收、儲存、驗收測試及庫存管理。 1.6.2.2 試劑與耗材 – 接收與儲存 – 當實驗室不是接收單位,應查證接收場所有適當的儲存與處理能力,以維持採購品項,避免損壞或變質的方式。 – 實驗室應依據製造商規格,儲存接收的試劑與耗材。 1.6.2.3 試劑與耗材 – 驗收測試 – 每個變更試劑或程序的新配方試劑組,或新批號或新進貨,應在檢測使用前加以查證其性能。 – 會影響檢測品質的耗材,應在檢測使用前加以查證其性能。 1.6.2.4 試劑與耗材 – 庫存管理 – 實驗室應建立試劑與耗材的庫存管制系統。 – 庫存管制系統應可區隔尚未查證、不可接受及已接受可供使用的試劑與耗材。 1.6.2.5 試劑與耗材 – 使用說明 – 試劑與耗材的使用說明,包括製造商所提供的,應可隨時取閱。 1.6.2.6 試劑與耗材 – 不良事件通報 – 不良事件與意外事故可直接歸咎於特定試劑與耗材時,應加以調查。當有要求時,通報製造商與適當權責機關。 1.6.2.7 試劑與耗材 – 紀錄 – 對檢測的性能有關的每項試劑與耗材,應維持其紀錄。這些紀錄應包括,但不限於下列: a)試劑與耗材的識別; b)製造商名稱與批次碼或批號; c)供應商或製造商的連絡資訊; d)接收日期、效期,加入服務的日期,當可行時,材料停止服務的日期; e)接收時的條件(例如接受或損壞); f)製造商的說明; g)證實試劑與耗材於初始可接受使用的紀錄; h)確認試劑與耗材可持續接受使用的性能紀錄; – 當實驗室使用自行配製或完全自行開發的試劑時,紀錄應除包括上述相關資訊外,還有提及配製人員與配製日期。 | 5.3.2 Reagents and consumables 5.3.2.1 General The laboratory shall have a documented procedure for the reception, storage, acceptance testing and inventory management of reagents and consumables. 5.3.2.2 Reagents and consumables – Reception and storage Where the laboratory is not the receiving facility, it shall verify that the receiving location has adequate storage and handling capabilities to maintain purchased items in a manner that prevents damage or deterioration. The laboratory shall store received reagents and consumables according to manufacturer’s specifications. 5.3.2.3 Reagents and consumables – Acceptance testing Each new formulation of examination kits with changes in reagents or procedure, or a new lot or shipment, shall be verified for performance before use in examinations. Consumables that can affect the quality of examinations shall be verified for performance before use in examinations. 5.3.2.4 Reagents and consumables – Inventory management The laboratory shall establish an inventory control system for reagents and consumables. The system for inventory control shall segregate uninspected and unacceptable reagents and consumables from those that have been accepted for use. 5.3.2.5 Reagents and consumables – Instructions for use Instructions for the use of reagents and consumables, including those provided by the manufacturers, shall be readily available. 5.3.2.6 Reagents and consumables – Adverse incident reporting Adverse incidents and accidents that can be attributed directly to specific reagents or consumables shall be investigated and reported to the manufacturer and appropriate authorities, as required. 5.3.2.7 Reagents and consumables – Records Records shall be maintained for each reagent and consumable that contributes to the performance of examinations. These records shall include but not be limited to the following: a)identity of the reagent or consumable; b)manufacturer’s name and batch code or lot number; c)contact information for the supplier or the manufacturer; d)date of receiving, the expiry date, date of entering into service and, where applicable, the date the material was taken out of service; e)condition when received(e.g. acceptable or damaged); f)manufacturer’s instructions; g)records that confirmed the reagent’s or consumable’s initial acceptance for use; h)performance records that confirm the reagent’s or consumable’s ongoing acceptance for use. Where the laboratory uses reagents prepared or completed in-house, the records shall include, in addition to the relevant information above, reference to the person or persons undertaking their preparation and the date of preparation. |
建議符合方式:
用《設備、試劑及耗材管理程序》去規範試劑與耗材的接收、儲存、驗收,甚至庫存管理也可以寫在這本二階程序書中,而不良事件通報還是統一依循《不符合事件管理程序》處置。紀錄管理則可以規範在《設備、試劑及耗材管理程序》及《文件與紀錄管理程序》。
8.2 管理要求
組織與管理階層職責
實驗室應確保執行業務時符合本指引,且須為負法律責任之實體。應設置實驗室主管、品質主管等管理階層,並明訂其職責,且訂定倫理行為。
| LDTs 查核基準 | ISO 15189:2012,4.1 |
|---|---|
| 2.1 組織與管理階層職責 2.1.1 組織 2.1.1.1 概述 – 實驗室於固有設施或關聯或移動式設施執行作業時,應符合本查核基準要求。 2.1.1.2 法律實體 – 實驗室或其所屬的組織,應為對其所有作業活動負法律責任之實體。 2.1.1.3 倫理行為(Ethical conduct) – 實驗室管理階層應有妥善安排,以確保下列事項: a)不可涉及任何可能降低實驗室能力、公正性、判斷力或作業誠信的信心之任何活動; b)管理階層與人員能免於任何可能不利於其工作品質的不當商務、財務或其他壓力與影響; c)當可能存在競爭利益的潛在衝突時,應予以公開與適當地揭露; d)有適當程序以確保員工依據相關法規要求處理檢體; e)機密性資料的維持。 2.1.1.4 實驗室主管 – 實驗室應由有能力且被授予職責的人員(一人或多人)來領導管理其所提供的服務。 – 實驗室主管的職責應包括與實驗室所提供服務相關的專業、科學、諮詢或組織的、行政的及教育的事務。 – 實驗室主管可挑選適當任務及 / 或責任授予合格人員;惟實驗室主管仍應承擔實驗室整體運作與行政事務的最終責任。 – 實驗室主管的任務與職責應予以文件化。 – 實驗室主管(或被授予任務的指定人員)應具備必要的能力、職權及資源,以達成本查核基準要求。 – 實驗室主管(或指定人員)應: a)根據機構內的職責分工,提供實驗室服務的有效領導,包括預算計畫與財務管理; b)當有需求時,與相關認證與法規機關、合適的行政機關、健康照護團體、實驗室服務使用者以及有正式協議的供應商間,建立有效的實質關係; c)確保具有足夠學歷、訓練及能力的適當數量的員工,以提供符合使用者需求與要求的實驗室服務; d)確保品質政策的實施; e)依據優良操作與合適的法規,導入安全的實驗室環境; g)評選並監控實驗室供應商; h)評選受委託實驗室並監控其服務品質(同時參見 4.2); i)提供實驗室員工專業發展方案與機會,以參與專業實驗室組織的科學性與其他活動; j)明訂、實施及監控服務表現的標準與實驗室服務或其它服務的品質改進; 附註:如果適當,可行時,可由所屬組織體制內的各項品質改進委員會進行。 k)監控實驗室執行的所有工作,以決定資訊有效產出; l)處理來自員工及/或實驗室服務使用者的任何抱怨、詢問或建議(同時參見 4.5,3.5.3 及 3.5.4); m)設計與實施應變計畫,以確保發生緊急情況或其它狀況的期間,而實驗室服務受限或無法提供時,仍可提供基本服務; 附註:應變計畫須定期予以測試演練。 n)適當時,計劃並指導研究與發展。 2.1.2 管理階層職責 2.1.2.1 管理階層承諾 – 實驗室管理階層應藉由下列各項,對品質管理系統發展與實施,以及持續改進其有效性之承諾,提供證據: a)與實驗室人員溝通符合使用者需求與要求(見 2.1.2.2)及法規與認證要求的重要性; b)建立品質政策(見 2.1.2.3); c)確保品質目標與計畫已予建立(見 2.1.2.4); d)明訂所有人員的職責、職權及相互關係(見 2.1.2.5); e)建立溝通流程(見 2.1.2.6); f)指派品質主管,無論其職稱(見 2.1.2.7); g)執行管理審查(見 3.6); h)確保所有人員均具備執行其受指派活動的能力(見 1.2.1); i)確保適當資源之備妥(見 1.5 及 1.6),以能適當執行檢測前、檢測中及檢測後的活動(見 5.1,5.2 及 5.4)。 2.1.2.2 使用者的需求 – 實驗室管理階層應確保實驗室服務,包括適當檢測建議與解釋服務,符合實驗室服務使用者的需求。(同時參見 4.1 與 3.5.3)。 2.1.2.3 品質政策 – 實驗室管理階層應在品質政策內明訂其品質管理系統的宗旨。實驗室管理階層應確保其品質政策: a)對組織之目的是適當的; b)包括關於優良專業操作、符合預期用途的檢測、遵照本查核基準要求及持續改進實驗室服務品質之承諾; c)提供一個建立與審查品質目標的架構; d)在組織內已予充份溝通與瞭解; e)對其持續適切性已予審查。 2.1.2.4 品質目標與規劃 – 實驗室管理階層應建立組織內相關部門與階層的品質目標,包括符合使用者需求與要求的必要內容。品質目標應可量測且與品質政策一致。實驗室管理階層應確保品質管理系統的規劃已予實施,以符合要求(見 2.2)與品質目標。 – 當規劃與實施品質管理系統變更時,實驗室管理階層應確保維持品質管理系統的完整性。 2.1.2.5 職責、職權及相互關係 – 實驗室管理階層應確保實驗室組織內部的職責、職權及相互關係,已予明訂、文件化及充份溝通。其應包括指派各實驗室部門的負責人員與指派重要管理與技術人員的代理。 附註:鑑於小型實驗室個別人員可能有多個職務,故每個職務都指定代理人可能不切實際。 2.1.2.6 溝通 – 實驗室管理階層應有與員工溝通的有效方式(同時參見 3.5.4)。在溝通與會議時討論事項之紀錄應予以維持。 – 實驗室管理階層應確保已建立實驗室與其利害關係者間適當溝通流程,並就有關實驗室檢測前、檢測中及檢測後流程及品質管理系統之有效性進行溝通。 2.1.2.7 品質主管 – 實驗室管理階層應指派一位具專業的人員擔任品質主管,不受其他職責所影響,授予下列職責與職權: a)確保品質管理系統所需的流程,已予建立、實施及維持; b)向具有決定實驗室政策、目標與資源之實驗室管理階層報告品質管理系統的績效與改進之任何需求; c)確保促進整個實驗室組織對使用者需求與要求之認知。 | 4.1 Organization and management responsibility 4.1.1 Organization 4.1.1.1 General The medical laboratory(hereinafter referred to as ‘the laboratory’)shall meet the requirements of this International Standard when carrying out work at its permanent facilities, or in associated or mobile facilities. 4.1.1.2 Legal entity The laboratory or the organization of which the laboratory is a part shall be an entity that can be held legally responsible for its activities. 4.1.1.3 Ethical conduct Laboratory management shall have arrangements in place to ensure the following: a)there is no involvement in any activities that would diminish confidence in the laboratory’s competence, impartiality, judgement or operational integrity; b)management and personnel are free from any undue commercial, financial, or other pressures and influences that may adversely affect the quality of their work; c)where potential conflicts in competing interests may exist, they shall be openly and appropriately declared; d)there are appropriate procedures to ensure that staff treat human samples, tissues or remains according to relevant legal requirements; e)confidentiality of information is maintained. 4.1.1.4 Laboratory director The laboratory shall be directed by a person or persons with the competence and delegated responsibility for the services provided. The responsibilities of the laboratory director shall include professional, scientific, consultative or advisory, organizational, administrative and educational matters relevant to the services offered by the laboratory. The laboratory director may delegate selected duties and/or responsibilities to qualified personnel; however, the laboratory director shall maintain the ultimate responsibility for the overall operation and administration of the laboratory. The duties and responsibilities of the laboratory director shall be documented. The laboratory director(or the designates for delegated duties)shall have the necessary competence, authority and resources in order to fulfil the requirements of this International Standard. The laboratory director(or designate/s)shall: a)provide effective leadership of the medical laboratory service, including budget planning and financial management, in accordance with institutional assignment of such responsibilities; b)relate and function effectively with applicable accrediting and regulatory agencies, appropriate administrative officials, the healthcare community, and the patient population served, and providers of formal agreements, when required; c)ensure that there are appropriate numbers of staff with the required education, training and competence to provide medical laboratory services that meet the needs and requirements of the users; d)ensure the implementation of the quality policy; e)implement a safe laboratory environment in compliance with good practice and applicable requirements; g)ensure the provision of clinical advice with respect to the choice of examinations, use of the service and interpretation of examination results; h)select and monitor laboratory suppliers; i)select referral laboratories and monitor the quality of their service(see also 4.5); j)provide professional development programmes for laboratory staff and opportunities to participate in scientific and other activities of professional laboratory organizations; k)define, implement and monitor standards of performance and quality improvement of the medical laboratory service or services; NOTE This may be done within the context of the various quality improvement committees of the parent organization, as appropriate, where applicable. l)monitor all work performed in the laboratory to determine that clinically relevant information is being generated; m)address any complaint, request or suggestion from staff and/or users of laboratory services(see also 4.8, 4.14.3 and 4.14.4); n)design and implement a contingency plan to ensure that essential services are available during emergency situations or other conditions when laboratory services are limited or unavailable; NOTE Contingency plans should be periodically tested. o)plan and direct research and development, where appropriate. 4.1.2 Management responsibility 4.1.2.1 Management commitment Laboratory management shall provide evidence of its commitment to the development and implementation of the quality management system and continually improve its effectiveness by: a)communicating to laboratory personnel the importance of meeting the needs and requirements of users(see 4.1.2.2)as well as regulatory and accreditation requirements; b)establishing the quality policy(see 4.1.2.3); c)ensuring that quality objectives and planning are established(see 4.1.2.4); d)defining responsibilities, authorities and interrelationships of all personnel(see 4.1.2.5); e)establishing communication processes(see 4.1.2.6); f)appointing a quality manager, however named(see 4.1.2.7); g)conducting management reviews(see 4.15); h)ensuring that all personnel are competent to perform their assigned activities(see 5.1.6); i)ensuring availability of adequate resources(see 5.1, 5.2 and 5.3)to enable the proper conduct of pre-examination, examination and post-examination activities(see 5.4, 5,5, and 5.7). 4.1.2.2 Needs of users Laboratory management shall ensure that laboratory services, including appropriate advisory and interpretative services, meet the needs of patients and those using the laboratory services.(see also 4.4 and 4.14.3). 4.1.2.3 Quality policyLaboratory management shall define the intent of its quality management system in a quality policy. Laboratory management shall ensure that the quality policy: a)is appropriate to the purpose of the organization; b)includes a commitment to good professional practice, examinations that are fit for intended use, compliance with the requirements of this International Standard, and continual improvement of the quality of laboratory services; c)provides a framework for establishing and reviewing quality objectives; d)is communicated and understood within the organization; e)is reviewed for continuing suitability. 4.1.2.4 Quality objectives and planning Laboratory management shall establish quality objectives, including those needed to meet the needs and requirements of the users, at relevant functions and levels within the organization. The quality objectives shall be measurable and consistent with the quality policy. Laboratory management shall ensure that planning of the quality management system is carried out to meet the requirements(see 4.2)and the quality objectives. Laboratory management shall ensure that the integrity of the quality management system is maintained when changes to the quality management system are planned and implemented. 4.1.2.5 Responsibility, authority and interrelationships Laboratory management shall ensure that responsibilities, authorities and interrelationships are defined, documented and communicated within the laboratory organization. This shall include the appointment of person(s)responsible for each laboratory function and appointment of deputies for key managerial and technical personnel. NOTE It is recognized that in smaller laboratories individuals can have more than one function and that it could be impractical to appoint deputies for every function. 4.1.2.6 Communication Laboratory management shall have an effective means for communicating with staff(see also 4.14.4). Records shall be kept of items discussed in communications and meetings. Laboratory management shall ensure that appropriate communication processes are established between the laboratory and its stakeholders and that communication takes place regarding the effectiveness of the laboratory’s pre-examination, examination and post-examination processes and quality management system. 4.1.2.7 Quality manager Laboratory management shall appoint a quality manager who shall have, irrespective of other responsibilities, delegated responsibility and authority that includes: a)ensuring that processes needed for the quality management system are established, implemented, and maintained; b)reporting to laboratory management, at the level at which decisions are made on laboratory policy, objectives, and resources, on the performance of the quality management system and any need for improvement; c)ensuring the promotion of awareness of users’ needs and requirements throughout the laboratory organization. |
建議符合方式:
《教育訓練與員工資格管理程序》規範新進人員教育訓練時,應教導員工「不可涉及任何可能降低實驗室能力、公正性、判斷力或作業誠信的信心之任何活動」等等,並且在《文件與紀錄管理程序》中定義機密文件,以及瀏覽權限、流通管制方式。
另外可用《合約管理程序》規範各式合約的審查流程與管理方式,以及用《檢體接收與處理管理程序》規定接收、處理檢體的細節。
關於機密性資料的管理規範寫在《文件與紀錄管理程序》,要是有機密性資料,例如檢驗紀錄、檢體資訊放在實驗室內,則可在《設施與環境維護程序》內規定門禁權限;合約、協議的制訂、審查、核准、修訂、廢止規定則依循《合約管理程序》。
將實驗室主管的任務與職責文件化在《組織權責與代理人程序》裡,並利用《教育訓練與員工資格管理程序》去確認其具備必要的能力、職權。
當提到評選供應商、受委託實驗室時,可將相關規定明訂於《供應商及採購管理程序》;《持續改進管理程序》中可明訂並監控各項品質紀錄、指標,以鑑定改進機會;應變計畫相關規定則可以訂於《應變管理程序》。
《客訴與回饋管理程序》可處理來自員工、實驗室服務使用者、客戶的任何抱怨、詢問或建議。最後,如同前面規劃的,所有不符合事件的處置方式都可以寫在《不符合事件管理程序》。
《查核基準》槓掉了 2.1.1.4.f)「確保提供關於檢測選擇、服務使用及檢測結果解釋的臨床建議」,當然也是因為台灣特色的 LDTs 的管理架構。但 ISO15189:2012 的 4.1.1.4.f) 章節規定:serve as a contributing member of the medical staff for those facilities served, if applicable and appropriate 直接似乎直接消失在《查核基準》中,而不是被槓掉。
品質管理系統
實驗室應有良好的品質管理系統,並應有品質手冊。
| LDTs 查核基準 | ISO 15189:2012,4.2 |
|---|---|
| 2.2 品質管理系統 2.2.1 一般要求 – 依本查核基準要求,實驗室應建立、文件化、實施及維持品質管理系統,並持續改進其有效性。 – 品質管理系統應提供全部所需完整的流程,以達成其品質政策與目標並符合使用者需求與要求。 – 實驗室應: a)決定此品質管理系統所需求的流程,並確保這些流程在整個實驗室之應用; b)決定這些流程的順序與相互作用; c)決定用以確保這些流程的運作與管制兩者均有效所需的準則與方法; d)確保用以支援此等流程的運作與監控所必要資源與資訊之備妥; e)監控與評估這些流程; f)實施用以達成流程所規劃的結果與持續改進這些流程所需必要措施。 2.2.2 文件化要求 2.2.2.1 概述 – 品質管理系統文件化應包括: a)品質政策(見 2.1.2.3)與品質目標(見 2.1.2.4)的文件化敘述; b)品質手冊(見 2.2.2.2); c)本查核基準所要求的程序與紀錄; d)實驗室為確保其流程有效規劃、運作與管制所決定的文件與紀錄(見 3.4); e)適用法規、標準及其他規範性文件的複本。 附註:文件能為任何形式或類型的媒體,可隨時提供取用與避免未經授權的更改及不當使用造成的毀損。 2.2.2.2 品質手冊 – 實驗室應建立與維持品質手冊,其包括: a)品質政策(見 2.1.2.3)或註明其出處; b)說明品質管理系統的範圍; c)敘述實驗室組織與管理結構及與任何母機構的隸屬關係; d)說明實驗室管理階層(包括實驗室主管與品質主管)的角色與職責,以確保符合本查核基準; e)說明於品質管理系統所使用的文件架構與關係; f)為品質管理系統與支援其涉及的管理與技術活動而建立之文件化政策。 – 所有實驗室人員應可取用並被教導使用與應用品質手冊與相關文件。 | 4.2 Quality management system 4.2.1 General requirements The laboratory shall establish, document, implement and maintain a quality management system and continually improve its effectiveness in accordance with the requirements of this International Standard. The quality management system shall provide for the integration of all processes required to fulfil its quality policy and objectives and meet the needs and requirements of the users. The laboratory shall: a)determine the processes needed for the quality management system and ensure their application throughout the laboratory; b)determine the sequence and interaction of these processes; c)determine criteria and methods needed to ensure that both the operation and control of these processes are effective; d)ensure the availability of resources and information necessary to support the operation and monitoring of these processes; e)monitor and evaluate these processes; f)implement actions necessary to achieve planned results and continual improvement of these processes. 4.2.2 Documentation requirements 4.2.2.1 General The quality management system documentation shall include: a)statements of a quality policy(see 4.1.2.3)and quality objectives(see 4.1.2.4); b)a quality manual(see 4.2.2.2); c)procedures and records required by this International Standard; d)documents, and records(see 4.13), determined by the laboratory to ensure the effective planning, operation and control of its processes; e)copies of applicable regulations, standards and other normative documents. NOTE The documentation can be in any form or type of medium, providing it is readily accessible and protected from unauthorized changes and undue deterioration. 4.2.2.2 Quality manual The laboratory shall establish and maintain a quality manual that includes: a)the quality policy(see 4.1.2.3)or makes reference to it; b)a description of the scope of the quality management system; c)a presentation of the organization and management structure of the laboratory and its place in any parent organization; d)a description of the roles and responsibilities of laboratory management(including the laboratory director and quality manager)for ensuring compliance with this International Standard; e)a description of the structure and relationships of the documentation used in the quality management system; f)the documented policies established for the quality management system and reference to the managerial and technical activities that support them. All laboratory staff shall have access to and be instructed on the use and application of the quality manual and the referenced documents. |
建議符合方式:
可在《品質手冊》放一張二階程序書與 LDTs 查核基準對照表,展現決定品質管理系統所需求的流程,並且沒有缺漏。同時,在《品質手冊》放入二階程序書的流程圖,以說明品質管理系統的順序與相互關係。還必須在《品質手冊》中寫清楚 2.2.2.2 章節規定的那 6 點。
在《品質管理系統規劃程序》裡面說明一下品質管理系統的重點,例如:要制訂品質政策,及如何、何時建立品質目標,還有要指定實驗室負責人與專任品質主管等等。利用定期的《管理審查管理程序》確保備妥所有流程的運作與監控所必要資源與資訊。
「確保其流程有效規劃、運作與管制所決定的文件與紀錄」就用《文件與紀錄管理程序》來實現。
所有文件可以放在雲端空間,讓相關人員隨時取閱。記得要設定唯讀權限,避免「未經授權的更改及不當使用造成的毀損」。
在《教育訓練與員工資格管理程序》中規定所有新進人員都要被教導如何使用《品質手冊》及其他二、三文件及四階表單。
最後,利用《持續改進管理程序》監控與評估所有關鍵流程,並實施持續改進這些流程所需必要措施。
文件管制
實驗室應有文件化程序及保存,且能有系統的妥善管理。
| LDTs 查核基準 | ISO 15189:2012,4.3 |
|---|---|
| 2.3 文件管制 – 實驗室應管制品質管理系統所需的文件,並應確保防止任何過期文件被誤用。 附註 1:文件管制須考量該文件會隨版本或時間而更動。舉例包括政策聲明、使用說明、流程圖、程序、規格、格式、校正表、生物參考區間及其來源、圖表、圖片、公告、備忘錄、軟體文件、圖稿、計畫、合約及檢測程序所引用的外部文件如法規,標準及教科書等。 附註 2:紀錄包含從特定時間點取得的資訊,以說明活動達成的結果或提供執行活動完成的證據,並依據 3.4 紀錄管制要求加以維持。 – 實驗室應有文件化的程序,以確保符合下列情況: a)凡作為品質管理系統一部份而發行之所有文件,包括維持於電腦系統的文件,應於發行前經由被授權人員審查與核准。 b)所有文件應予以識別,以包括: – 文件名稱; – 每頁的唯一識別; – 最新版本日期及/或版本編號; – 頁碼與總頁數(例如,「5 頁之 1」,「5 頁之 2」); – 發行之權責 附註:「版本」代表伴隨改變與修正在不同時期所發佈出版的次數。「版本」與「修訂 版或改編版」同義。 c)以文件清單(例如,文件登錄、日誌或主目錄)來識別最新被授權的版本與其分發狀況 。 d)在使用場所僅有最新授權版本文件可予取得。 e)當實驗室的文件化管制系統允許在文件再發行之前,可以手寫方式修正文件。實驗室應對此類修正之程序與權責加以明訂,此類修正應清楚地標明、簽署並標註日期,經修訂的文件應於指定時間內再發行。 f)對於文件的變更內容予以識別。 g)文件保持清晰易讀。 h)應定期審查與更新文件,以確保文件持續符合使用的目的。 i)過期的管制文件,予以註明廢止日期與註記。 j)於特定時間週期或符合適當的特定要求,至少保留一份過期管制文件複本。 | 4.3 Document control The laboratory shall control documents required by the quality management system and shall ensure that unintended use of any obsolete document is prevented. NOTE 1 Documents that should be considered for document control are those that may vary based on changes in versions or time. Examples include policy statements, instructions for use, flow charts, procedures, specifications, forms, calibration tables, biological reference intervals and their origins, charts, posters, notices, memoranda, software documentation, drawings, plans, agreements, and documents of external origin such as regulations, standards and text books from which examination procedures are taken. NOTE 2 Records contain information from a particular point in time stating results achieved or providing evidence of activities performed and are maintained according to the requirements given in 4.13, Control of records. The laboratory shall have a documented procedure to ensure that the following conditions are met. a)All documents, including those maintained in a computerized system, issued as part of the quality management system are reviewed and approved by authorized personnel before issue. b)All documents are identified to include: – a title; – a unique identifier on each page; – the date of the current edition and/or edition number; – page number to total number of pages(e.g. “Page 1 of 5,” “Page 2 of 5,”); – authority for issue. NOTE ‘Edition’ is used to mean one of a number of printings issued at separate times that incorporates alterations and amendments. ‘Edition’ can be regarded as synonymous with ‘revision or version’. c)Current authorized editions and their distribution are identified by means of a list(e.g. document register, log or master index). d)Only current, authorized editions of applicable documents are available at points of use. e)Where a laboratory’s document control system allows for the amendment of documents by hand, pending the re-issue of documents, the procedures and authorities for such amendments are defined, amendments are clearly marked, initialled and dated, and a revised document is issued within a specified time period. f)Changes to documents are identified. g)Documents remain legible. h)Documents are periodically reviewed and updated at a frequency that ensures that they remain fit for purpose. i)Obsolete controlled documents are dated and marked as obsolete. j)At least one copy of an obsolete controlled document is retained for a specified time period or in accordance with applicable specified requirements. |
建議符合方式:
這邊所有規定細節都可以明訂在《文件與紀錄管理程序》,記得要建立「文件清單」,一般稱為《文件總覽表》。
8.3 品質要求
不符合事件的鑑別與管制
實驗室有責任進行監控程序,並將其流程文件化,以鑑別與管理整個檢測過程任何與品質管理系統相關的「不符合事件」。
| LDTs 查核基準 | ISO 15189:2012,4.9 |
|---|---|
| 3.1 不符合事件的鑑別與管制 – 實驗室應有文件化的程序,以鑑別與管理任何與品質管理系統相關的不符合事件,包括檢測前、檢測中或檢測後的流程。 – 此程序應確保: a)指派處理不符合事件的權責人員; b)明訂擬採取的立即措施; c)決定不符合事件的影響程度; d)必要時,暫停檢測與留置檢測結果單; e)任何不符合的檢測事件應考慮其影響。當適當時,通知申請者或被授權使用該份結果的負責人員; f)必要時,應召回或適當地識別已釋出任何不符合或潛在不符合的檢測結果; g)界定授權檢測工作再開始之權責; h)每一不符合事件予以文件化與記錄,於特定期間審查,以偵測其發展趨勢,並導入初步矯正措施。 附註:不符合的檢測事件或活動可發生於許多不同方面,可經由不同途徑如臨床醫師的抱怨、內部品質管制指標、儀器校正、消耗性材料查核、實驗室間比對、員工意見、檢 測結果單與憑證的查核、實驗室管理審查、及內部與外部稽核等。 – 如果判定檢測前、檢測中及檢測後流程的不符合事件可能再發生,或對實驗室符合本身程序有懷疑時,實驗室應採取措施以鑑別、文件化及消除原因。擬採行的矯正措施應予以決定與文件化(見 3.2.1)。 | 4.9 Identification and control of nonconformities The laboratory shall have a documented procedure to identify and manage nonconformities in any aspect of the quality management system, including pre-examination, examination or post-examination processes. The procedure shall ensure that: a)the responsibilities and authorities for handling nonconformities are designated; b)the immediate actions to be taken are defined; c)the extent of the nonconformity is determined; d)examinations are halted and reports withheld as necessary; e)the medical significance of any nonconforming examinations is considered and, where appropriate, the requesting clinician or authorized individual responsible for using the results is informed; f)the results of any nonconforming or potentially nonconforming examinations already released are recalled or appropriately identified, as necessary; g)the responsibility for authorization of the resumption of examinations is defined; h)each episode of nonconformity is documented and recorded, with these records being reviewed at regular specified intervals to detect trends and initiate corrective action. NOTE Nonconforming examinations or activities occur in many different areas and can be identified in many different ways, including clinician complaints, internal quality control indications, instrument calibrations, checking of consumable materials, interlaboratory comparisons, staff comments, reporting and certificate checking, laboratory management reviews, and internal and external audits. When it is determined that nonconformities in pre-examination, examination and post-examination processes could recur or that there is doubt about the laboratory’s compliance with its own procedures, the laboratory shall take action to identify, document and eliminate the cause(s). Corrective action to be taken shall be determined and documented(see 4.10). |
建議符合方式:
如同前面說的,所有不符合事件都可以匯入《不符合事件管理程序》來處置與記錄。
矯正與預防措施
實驗室應制定不符合事件處理之標準作業程序,包括消除不符合事件的肇因,並制定與採行預防措施 ,以避免潛在的不符合事件。
| LDTs 查核基準 | ISO 15189:2012,4.10 – 4.11 |
|---|---|
| 3.2 矯正與預防措施 3.2.1 矯正措施(Corrective action) – 實驗室應採取矯正措施,以消除不符合事件的原因。矯正措施應與所遭遇不符合事件之影響相稱。 – 實驗室應有文件化的程序,以: a)審查不符合事件; b)決定不符合事件的根本原因; c)評估矯正措施的需求,以確保不符合事件不再發生; d)決定與實施所需的矯正措施; e)記錄所採行的矯正措施的結果(見 3.4); f)審查所採行矯正措施的有效性(見 3.5.5)。 附註:發生不符合事件時,為減輕其立即影響所採取的措施,可視為「立即」措施。只有在移除造成不符合事件問題的根本原因,所採取的措施,才可視為「矯正」措施。 3.2.2 預防措施(Preventive action) – 實驗室應決定措施,以消除潛在不符合事件之原因,以防止其發生。預防措施應與潛在問題之影響相稱。 – 實驗室應有文件化的程序,以: a)審查實驗室資料與資訊,以決定那些潛在不符合事件的存在; b)決定潛在不符合事件的根本原因; c)評估預防措施之需求,以預防不符合事件之發生; d)決定與實施所需的預防措施; e)記錄所採行預防措施的結果(見 3.4); f)審查所採行預防措施的有效性。 附註:預防措施是事先行動流程以鑑別改進機會,而不是對問題或抱怨(舉例如不符合事件)鑑別後的一種反應。除了審查作業程序外,預防措施可涉及分析資料,包括趨勢與風險分析及外部品質評鑑(能力試驗)。 | 4.10 Corrective action The laboratory shall take corrective action to eliminate the cause(s)of nonconformities. Corrective actions shall be appropriate to the effects of the nonconformities encountered. The laboratory shall have a documented procedure for: a)reviewing nonconformities; b)determining the root causes of nonconformities; c)evaluating the need for corrective action to ensure that nonconformities do not recur; d)determining and implementing corrective action needed; e)recording the results of corrective action taken(see 4.13); f)reviewing the effectiveness of the corrective action taken(see 4.14.5). NOTE Action taken at the time of the nonconformity to mitigate its immediate effects is considered “immediate” action. Only action taken to remove the root cause of the problem that is causing the nonconformities is considered “corrective” action. 4.11 Preventive action The laboratory shall determine action to eliminate the causes of potential nonconformities in order to prevent their occurrence. Preventive actions shall be appropriate to the effects of the potential problems. The laboratory shall have a documented procedure for: a)reviewing laboratory data and information to determine where potential nonconformities exist; b)determining the root cause(s)of potential nonconformities; c)evaluating the need for preventive action to prevent the occurrence of nonconformities; d)determining and implementing preventive action needed; e)recording the results of preventive action taken(see 4.13); f)reviewing the effectiveness of the preventive action taken. NOTE Preventive action is a proactive process for identifying opportunities for improvement rather than a reaction to the identification of problems or complaints(i.e. nonconformities). In addition to review of the operational procedures, preventive action might involve analysis of data, including trend and risk analyses and external quality assessment(proficiency testing). |
建議符合方式:
「矯正措施」是針對「已發生」的不符合事件的根本原因去對症下藥,避免「再發生」(亡羊補牢),所以可以單純用《不符合事件管理程序》去處理。但「預防措施」是針對「潛在、可能、且尚未發生」問題的根本原因,避免這個問題真的「發生」(防範未然),這一般必須透過監控關鍵流程,從各個參數中找出有問題的趨勢。所以,可以建立《持續改進管理程序》,利用此二階程序書去監控、取得關鍵流程參數,用以判斷是否有不正常的趨勢,以決定是否要啟動預防措施。
持續改進
實驗室應制定改進計畫和相關目標,持續的改善與增進監測品質。
| LDTs 查核基準 | ISO 15189:2012,4.12 |
|---|---|
| 3.3 持續改進 – 實驗室應持續改進品質管理系統的有效性,包括檢測前、檢測中及檢測後流程,經由管理審查將實驗室之評估活動、矯正措施與預防措施的實際執行成效,與所聲明預期的品質政策與品質目標相互比較。應針對風險評鑑(risk assessment)所列為最高優先範圍進行改進活動。適當時,改進行動計畫應予以展開、文件化及實施。已採取措施的有效性,應經由重點審查或關切範圍的稽核予以決定(同時參見 3.5.5)。 – 實驗室管理階層應確保實驗室品質之持續改進活動。 – 當此持續改進方案鑑別出有改進的機會,不論其發生於何處,實驗室管理階層應予提出。實驗室管理階層應就改進計畫和相關目標與員工溝通。 | 4.12 Continual improvement The laboratory shall continually improve the effectiveness of the quality management system, including the pre-examination, examination and post-examination processes, through the use of management reviews to compare the laboratory’s actual performance in its evaluation activities, corrective actions and preventive actions with its intentions, as stated in the quality policy and quality objectives. Improvement activities shall be directed at areas of highest priority based on risk assessments. Action plans for improvement shall be developed, documented and implemented, as appropriate. The effectiveness of the actions taken shall be determined through a focused review or audit of the area concerned(see also 4.14.5). Laboratory management shall ensure that the laboratory participates in continual improvement activities that encompass relevant areas and outcomes of patient care. When the continual improvement programme identifies opportunities for improvement, laboratory management shall address them regardless of where they occur. Laboratory management shall communicate to staff improvement plans and related goals. |
建議符合方式:
利用《持續改進管理程序》去鑑別改善機會,找出可能的問題後,導入《不符合事件管理程序》處理、追蹤及記錄,再由《管理審查管理程序》評估各項措施的實際執行成效,並與所聲明預期的品質政策與品質目標相互比較。
另外,還要建立《風險管理程序》,以找出並控制風險。
紀錄管制
實驗室於鑑別、收集、索引、取閱、儲存、維持、修正及安全棄置品質與技術紀錄,皆需建立文件化之程序。
| LDTs 查核基準 | ISO 15189:2012,4.13 |
|---|---|
| 3.4 紀錄管制 – 實驗室應有文件化的程序,以鑑別、收集、索引、取閱、儲存、維持、修正及安全棄置品質與技術紀錄。 – 執行影響檢測品質的每項活動應即時建立紀錄。 附註 1:紀錄能為任何形式或類型的媒體,可隨時提供取用與避免未經授權的更改。 – 紀錄修正的日期與時間(當有關聯時),應連同修正人員的識別一併留存。 – 實驗室應明訂與品質管理系統相關,包括檢測前、檢測中及檢測後流程等各類紀錄的保存期間。 – 紀錄依分類可有不同保存期限。然而,已發放的檢測結果,若與醫療相關或有法規要求時,應可予以取用。 附註 2:某類程序(例如組織學檢測、遺傳檢測、小兒科檢測)與法律責任有相關,此等紀錄之保留可比其他紀錄期限更長。 – 機構應提供適當儲存紀錄的環境,以避免損毀、遺失或未經授權取得(見 1.5.6)。 附註 3:對某些紀錄,特別是電子式儲存者,最安全儲存方式可以是有安全防護的媒體與異地備援。 – 紀錄至少應包括下列事項: a)供應商的選擇與其服務表現及認可供應商名單的變更; b)員工資格、訓練及能力紀錄; c)檢測的申請; d)實驗室接收樣本的紀錄; e)檢測用之試劑與材料資訊(例如,批號文件、供應憑證、包裝內附說明); f)實驗室工作簿或工作單; g)儀器列印的資料、保存的資料及資訊; h)檢測結果; i)儀器保養紀錄,包括內部與外部校正紀錄; j)校正功能與轉換係數; k)品質管制紀錄; l)事件紀錄與已採取措施; m)事故紀錄與已採取措施; n)風險管理紀錄; o)鑑別的不符合事件與已採取之立即或矯正措施; p)已採取的預防措施; q)抱怨與已採取措施; r)內部與外部稽核紀錄; s)實驗室間比對的檢測結果; t)品質改進活動的紀錄; u)記載有關實驗室品質管理活動決策的會議紀錄; v)管理審查紀錄; – 所有以上品質與技術紀錄,應可於實驗室管理審查時取得(見 4.15)。 | 4.13 Control of records The laboratory shall have a documented procedure for identification, collection, indexing, access, storage, maintenance, amendment and safe disposal of quality and technical records. Records shall be created concurrently with performance of each activity that affects the quality of the examination. NOTE 1 Records can be in any form or type of medium providing they are readily accessible and protected from unauthorized alterations. The date and, where relevant, the time of amendments to records shall be captured along with the identity of personnel making the amendments(see 5.8.6). The laboratory shall define the time period that various records pertaining to the quality management system, including pre-examination, examination and post-examination processes, are to be retained. The length of time that records are retained may vary; however, reported results shall be retrievable for as long as medically relevant or as required by regulation. NOTE 2 Legal liability concerns regarding certain types of procedures(e.g. histology examinations, genetic examinations, paediatric examinations)may require the retention of certain records for much longer periods than for other records. Facilities shall provide a suitable environment for storage of records to prevent damage, deterioration, loss or unauthorized access(see 5.2.6). NOTE 3 For some records, especially those stored electronically, the safest storage may be on secure media and an offsite location(see 5.9.4). Records shall include, at least, the following: a)supplier selection and performance, and changes to the approved supplier list; b)staff qualifications, training and competency records; c)request for examination; d)records of receipt of samples in the laboratory; e)information on reagents and materials used for examinations(e.g. lot documentation, certificates of supplies, package inserts); f)laboratory work books or work sheets; g)instrument printouts and retained data and information; h)examination results and reports; i)instrument maintenance records, including internal and external calibration records; j)calibration functions and conversion factors; k)quality control records; l)incident records and action taken; m)accident records and action taken; n)risk management records; o)nonconformities identified and immediate or corrective action taken; p)preventive action taken; q)complaints and action taken; r)records of internal and external audits; s)interlaboratory comparisons of examination results; t)records of quality improvement activities; u)minutes of meetings that record decisions made about the laboratory’s quality management activities; v)records of management reviews. All of these quality and technical records shall be available for laboratory management review(see 4.15). |
建議符合方式:
《文件與紀錄管理程序》可用來符合大部分的要求,但如果有很多電子檔案,可以利用《設備軟體與資訊系統維護程序》來管理,而如果是實驗室現場的文件、紀錄,則可搭配《設施與環境維護程序》來規範相關人員產出相關紀錄。
《特管辦法》第 39 條有明確規定:「施行實驗室開發檢測之認證實驗室,應依醫師開立之醫囑及其通過認證之檢測項目提供服務,並製作相關紀錄及出具檢測報告;其紀錄及報告,至少保存七年。」
評估與稽核
實驗室應規劃與實施所需之評估與內部稽核流程,以符合檢測服務之需求、品質系統之要求與改進之有效性。
| LDTs 查核基準 | ISO 15189:2012,4.14 |
|---|---|
| 3.5 評估與稽核 3.5.1 概述 – 實驗室應規劃與實施所需之評估與內部稽核流程,以: a)展示檢測前、檢測中與檢測後以及支援流程的方式於使用者需求與要求之符合性; b)確保品質管理系統之符合性; c)持續改進品質管理系統之有效性。 – 評估與改進活動的結果,應予納入管理審查(見 3.6)。 附註:相關改進活動,參見 3.2.1,3.2.2 及 3.3。 3.5.2 定期審查檢測申請以及程序與樣本要求的適當性 – 被授權的人員應定期審查實驗室所提供的檢測,以確保受理的檢測申請適用於申請者之需求。 – 實驗室應定期審查其所適用樣本類型的體積及品質要求,以確保無採檢不足或超量情形,及樣本已適當的採集以保存待測物。 3.5.3 使用者回饋的評估 – 實驗室應尋找有關使用者認知感受的訊息,如服務是否符合使用者需求與要求。 – 在實驗室可確保對其他使用者保密的條件下,取得與使用此訊息的方法應包括與使用者或其代表合作,以監控實驗室服務表現。已收集的訊息與採行措施的紀錄應予以維持。 3.5.4 員工建議 – 實驗室管理階層應鼓勵員工提供改進實驗室服務之任何方面的建議。此等建議應經評估,適當時加以實施並將結果回饋給員工。此等建議與管理階層採行措施的紀錄,應予維持。 3.5.5 內部稽核 – 實驗室應在計畫的週期內執行內部稽核,以決定品質管理系統內的所有活動,包括檢測前、檢測中及檢測後,是否: a) 符合本查核基準的要求與實驗室建立的要求,及 b)加以實施、有效及維持。 附註 1:內部稽核的週期一般須於一年內完成。內部稽核不需每一年全面涵蓋品質管理系統的所有要素。 – 實驗室可決定將特定活動列為重點,而未完全忽略其他要素。 – 稽核應由受過訓練人員執行,以評估品質管理系統的管理與技術流程的服務表現。稽核方案應考量到流程的現況與重要性,與擬受稽核的技術與管理的區域。稽核準則、範圍、頻率及方法應予以明訂與文件化。 – 稽核員的遴選與稽核的執行,應確保稽核流程的客觀性與公正性。在資源許可的情況下,稽核員應獨立於所擬稽核的活動。 附註 2:指引可參考 ISO 19011。 – 實驗室應有文件化的程序,以明訂稽核的規劃與執行、發放檢測結果及紀錄維持之職責與要求(見 3.4)。 – 當不符合事件已鑑別時,受稽核區域職責人員應確保立即採行適當的措施。採取的矯正措施應無不當延誤,以消除所偵查出之不符合事件的原因。(見 3.2.1) 3.5.6 風險管理 – 實驗室應針對影響安全的工作流程與檢測結果之潛在失效的衝擊進行評估,並應調整流程以減少或消除已鑑別的風險,並將決定及採行措施予以文件化。 3.5.7 品質指標 – 實驗室應建立品質指標,以監控與評估檢測前、檢測中及檢測後流程中各關鍵構面的表現。 舉例:不合格樣本的件數、簽收及/或接收錯誤的件數、檢測結果單修正的件數。品質指標的監控流程應加以規劃,內容包括建立目標、方法、說明、限制、行動計畫及量測期間。 – 這些指標應定期加以審查,以確保其持續的合適性。 附註:對於非檢測程序的品質指標監控,例如實驗室安全與環境,設備完備與人員紀錄,以及文件管制系統的有效性等,可提供有價值的管理見解。 – 實驗室在諮詢使用者後,應建立每項檢測項目的檢測結果完成時間,並可反應送檢單位之需求。實驗室應定期評估檢測結果單完成時間,不論其是否符合所建立的檢測結果單完成時間。 3.5.8 外部組織的審查 – 當由外部組織的審查指出實驗室有不符合事件或潛在不符合事件時,實驗室應採取適當的立即措施,與適當時的矯正措施或預防措施,以確保持續符合本查核基準的要求。外部組織的審查、採取的矯正措施及預防措施的紀錄應予以維持。 附註:外部認證組織的審查,舉例包括:認證評鑑、法規機關的訪查、以及衛生與安全訪查。 | 4.14 Evaluation and audits 4.14.1 General The laboratory shall plan and implement the evaluation and internal audit processes needed to: a)demonstrate that the pre-examination, examination and post-examination and supporting processes are being conducted in a manner that meets the needs and requirements of users; b)ensure conformity to the quality management system; c)continually improve the effectiveness of the quality management system. The results of evaluation and improvement activities shall be included in the input to the management review(see 4.15). NOTE For improvement activities, see 4.10, 4.11, and 4.12. 4.14.2 Periodic review of requests, and suitability of procedures and sample requirements Authorized personnel shall periodically review the examinations provided by the laboratory to ensure that they are clinically appropriate for the requests received. The laboratory shall periodically review its sample volume, collection device and preservative requirements for blood, urine, other body fluids, tissue and other sample types, as applicable, to ensure that neither insufficient nor excessive amounts of sample are collected and the sample is properly collected to preserve the measurand. 4.14.3 Assessment of user feedback The laboratory shall seek information relating to user perception as to whether the service has met the needs and requirements of users. The methods for obtaining and using this information shall include cooperation with users or their representatives in monitoring the laboratory’s performance, provided that the laboratory ensures confidentiality to other users. Records shall be kept of information collected and actions taken. 4.14.4 Staff suggestions Laboratory management shall encourage staff to make suggestions for the improvement of any aspect of the laboratory service. Suggestions shall be evaluated, implemented as appropriate and feedback provided to the staff. Records of suggestions and action taken by the management shall be maintained. 4.14.5 Internal audit The laboratory shall conduct internal audits at planned intervals to determine whether all activities in the quality management system, including pre-examination, examination, and post-examination: a)conform to the requirements of this International Standard and to requirements established by the laboratory, and b)are implemented, effective, and maintained. NOTE 1 The cycle for internal auditing should normally be completed in one year. It is not necessary that internal audits cover each year, in depth, all elements of the quality management system. The laboratory may decide to focus on a particular activity without completely neglecting the others. Audits shall be conducted by personnel trained to assess the performance of managerial and technical processes of the quality management system. The audit programme shall take into account the status and importance of the processes and technical and management areas to be audited, as well as the results of previous audits. The audit criteria, scope, frequency and methods shall be defined and documented. Selection of auditors and conduct of audits shall ensure objectivity and impartiality of the audit process. Auditors shall, wherever resources permit, be independent of the activity to be audited. NOTE 2 See ISO 19011 for guidance. The laboratory shall have a documented procedure to define the responsibilities and requirements for planning and conducting audits, and for reporting results and maintaining records(see 4.13). Personnel responsible for the area being audited shall ensure that appropriate action is promptly undertaken when nonconformities are identified. Corrective action shall be taken without undue delay to eliminate the causes of the detected nonconformities(see 4.10). 4.14.6 Risk management The laboratory shall evaluate the impact of work processes and potential failures on examination results as they affect patient safety, and shall modify processes to reduce or eliminate the identified risks and document decisions and actions taken. 4.14.7 Quality indicators The laboratory shall establish quality indicators to monitor and evaluate performance throughout critical aspects of pre-examination, examination and post-examination processes. EXAMPLE Number of unacceptable samples, number of errors at registration and/or accession, number of corrected reports. The process of monitoring quality indicators shall be planned, which includes establishing the objectives, methodology, interpretation, limits, action plan and duration of measurement. The indicators shall be periodically reviewed, to ensure their continued appropriateness. NOTE 1 Quality indicators to monitor non-examination procedures, such as laboratory safety and environment, completeness of equipment and personnel records, and effectiveness of the document control system may provide valuable management insights. NOTE 2 The laboratory should establish quality indicators for systematically monitoring and evaluating the laboratory’s contribution to patient care(see 4.12). The laboratory, in consultation with the users, shall establish turnaround times for each of its examinations that reflect clinical needs. The laboratory shall periodically evaluate whether or not it is meeting the established turnaround times. 4.14.8 Reviews by external organizations When reviews by external organizations indicate the laboratory has nonconformities or potential nonconformities, the laboratory shall take appropriate immediate actions and, as appropriate, corrective action or preventive action to ensure continuing compliance with the requirements of this International Standard. Records shall be kept of the reviews and of the corrective actions and preventive actions taken. NOTE Examples of reviews by external accreditation organizations include: accreditation assessments, regulatory agencies’ inspections, and health and safety inspections. |
建議符合方式:
在《稽核管理程序》中明訂內、外部稽核的處理方式,稽核發現的不符合事項可以利用《不符合事件管理程序》管理。另外,透過《客訴與回饋管理程序》及《持續改進管理程序》兩本二階程序書搞定使用者回饋的評估、員工建議。
風險管理的規定當然就是明訂在《風險管理程序》。
可以在《品質管理系統規劃程序》中規定要建立品質指標,具體的品質指標與監控頻率、方式則明訂於《持續改進管理程序》。
最後,把所有審查的規定,包含稽核結果、相關改進活動、品質指標持續合適性等等,都規範在《管理審查管理程序》中。
管理審查
實驗室管理階層應於規劃期間內審查實驗室品質管理系統,以確保維持其適切性、充分性、有效性,以及能支持服務對象的需求。
| LDTs 查核基準 | ISO 15189:2012,4.15 |
|---|---|
| 3.6 管理審查 3.6.1 概述 – 實驗室管理階層應在規劃的期間內審查品質管理系統,以確保其持續的適切性、足夠性、有效性。 3.6.2 審查輸入 – 管理審查輸入應來自以下評估結果的資訊,至少包括: a)定期審查檢測申請以及程序與樣本要求的適當性(見 3.5.2); b)使用者回饋的評估(見 3.5.3); c)員工建議(見 3.5.4); d)內部稽核(見 3.5.5); e)風險管理(見 3.5.6); f)品質指標的使用(見 3.5.7); g)外部組織的審查(見 3.5.8); h)參與實驗室間比對方案的結果(PT/EQA)(見 5.3.3); i)抱怨的監控與解決(見 4.5); j)供應商的服務表現(見 4.3); k)不符合事件的鑑別與管制(見 3.1); l)持續改進的結果(見 3.3),包括矯正措施(見 3.2.1)與預防措施的現況(見3.2.2); m)來自先前管理審查之措施的跟催; n)可能影響品質管理系統工作量與範圍、人員及場所等變更; o)改進建議,包括技術要求。 3.6.3 審查活動 – 審查應分析輸入資訊的不符合事件原因、趨勢及型態,以指出流程中的問題。 – 此審查應包括品質管理系統(含品質政策與品質目標)的改進機會與變更需求之評估。 3.6.4 審查輸出 管理審查期間來自於管理審查的輸出應納入紀錄,包含下列任何決定與措施: a)品質管理系統與其流程有效性之改進; b)對使用者服務的改進; c)資源需求。 附註:管理審查的時間間隔不得大於 12 個月;然而,當正在建構一個品質管理系統時,時間間隔可以縮短。 – 管理審查所發現與引發之措施,應予以記錄並告知實驗室人員。 – 實驗室管理階層應確保管理審查所引發措施,在明訂時限內完成。 | 4.15 Management review 4.15.1 General Laboratory management shall review the quality management system at planned intervals to ensure its continuing suitability, adequacy and effectiveness and support of patient care. 4.15.2 Review input The input to management review shall include information from the results of evaluations of at least the following: a)the periodic review of requests, and suitability of procedures and sample requirements(see 4.14.2); b)assessment of user feedback(see 4.14.3); c)staff suggestions(see 4.14.4); d)internal audits(see 4.14.5); e)risk management(see 4.14.6) f)use of quality indicators (see 4.14.7); g)reviews by external organizations (see 4.14.8); h)results of participation in interlaboratory comparison programmes(PT/EQA)(see 5.6.3); i)monitoring and resolution of complaints(see 4.8); j)performance of suppliers(see 4.6); k)identification and control of nonconformities(see 4.9); l)results of continual improvement(see 4.12)including current status of corrective actions(see 4.10)and preventive actions(see 4.11); m)follow-up actions from previous management reviews; n)changes in the volume and scope of work, personnel, and premises that could affect the quality management system; o)recommendations for improvement, including technical requirements. 4.15.3 Review activities The review shall analyse the input information for causes of nonconformities, trends and patterns that indicate process problems. This review shall include assessing these opportunities for improvement and the need for changes to the quality management system, including the quality policy and quality objectives. The quality and appropriateness of the laboratory’s contribution to patient care shall, to the extent possible, also be objectively evaluated. 4.15.4 Review output The output from the management review shall be incorporated into a record that documents any decisions made and actions taken during management review related to: a)improvement of the effectiveness of the quality management system and its processes; b)improvement of services to users; c)resource needs. NOTE The interval between management reviews should be no greater than 12 months; however, shorter intervals should be adopted when a quality management system is being established. Findings and actions arising from management reviews shall be recorded and reported to laboratory staff. Laboratory management shall ensure that actions arising from management review are completed within a defined timeframe. |
建議符合方式:
管理審查的規定當然就是寫在《管理審查管理程序》中囉。
我發現在《查核基準》 3.6.4 章節的附註中規定:「管理審查的時間間隔不『得』大於 12 個月」,ISO15189:2012 也是用代表 recommendation 的 should,而非用表示 requirement 的 shall。這表示其實管理審查間隔可以大於 12 個月。但一般來說,管理審查週期都是至少每 12 個月一次,如果要挑戰延長這個期限,可能需要準備一個好的理由來說服稽核員。
8.4 服務要求
服務協議
服務協議應文件化並定期審查,應考量申請及檢測結果之內容,協議應詳細指明申請所需資訊,以確保適當的檢測與結果呈現。
| LDTs 查核基準 | ISO 15189:2012,4.4 |
|---|---|
| 4.1 服務協議 4.1.1 服務協議的建立 – 實驗室應有文件化的程序,以建立與審查所提供之實驗室服務的協議。 – 實驗室所接受的每份檢測申請,應視為一種協議。 – 為提供實驗室服務的協議,應考量到申請內容、檢測及檢測結果單。協議應詳細指明申請所需資訊,以確保適當的檢測與結果解釋。 – 當實驗室依協議提供實驗室服務時,下列條件應加以滿足: a)顧客、使用者以及實驗室服務提供者的要求,包括擬採用的檢測流程,應加以明訂、文件化及予以瞭解(見 5.1.2 與 5.2)。 b)實驗室應有能力與資源來達成這些要求。 c)實驗室人員應有執行既定檢測之必要的專業技能與知識。 d)所選擇的檢測程序應適當且符合顧客的需求(見 5.2.1)。 e)與協議內容有差異且會影響檢測結果時,應通知顧客與使用者。 f)委託給受委託實驗室或顧問的任何工作,實驗室應予以註明。 4.1.2 服務協議的審查 – 實驗室服務的協議審查應包括所有協議細項。這些審查紀錄應包括任何協議的改變與任何相關的討論。 – 實驗室服務開始後,如果需修改協議,應重複執行相同的協議審查流程,且任何修正應與所有受影響的相關單位人員溝通。 | 4.4 Service agreements 4.4.1 Establishment of service agreements The laboratory shall have documented procedures for the establishment and review of agreements for providing medical laboratory services. Each request accepted by the laboratory for examination(s)shall be considered an agreement. Agreements to provide medical laboratory services shall take into account the request, the examination and the report. The agreement shall specify the information needed on the request to ensure appropriate examination and result interpretation. The following conditions shall be met when the laboratory enters into an agreement to provide medical laboratory services. a)The requirements of the customers and users, and of the provider of the laboratory services, including the examination processes to be used, shall be defined, documented and understood(see 5.4.2 and 5.5). b)The laboratory shall have the capability and resources to meet the requirements. c)Laboratory personnel shall have the skills and expertise necessary for the performance of the intended examinations. d)Examination procedures selected shall be appropriate and able to meet the customers’ needs(see 5.5.1). e)Customers and users shall be informed of deviations from the agreement that impact upon the examination results. f)Reference shall be made to any work referred by the laboratory to a referral laboratory or consultant. NOTE 2 Where patients are customers (e.g. when patients have the ability to directly request examinations), changes in service should be reflected in explanatory information and laboratory reports. NOTE 3 Laboratories should not enter into financial arrangements with referring practitioners or funding agencies where those arrangements act as an inducement for the referral of examinations or patients or interfere with the practitioner’s independent assessment of what is best for the patient. 4.4.2 Review of service agreements Reviews of agreements to provide medical laboratory services shall include all aspects of the agreement. Records of these reviews shall include any changes to the agreement and any pertinent discussions. When an agreement needs to be amended after laboratory services have commenced, the same agreement review process shall be repeated and any amendments shall be communicated to all affected parties. |
建議符合方式:
建立及審查合約的相關規定可以規範在《合約管理程序》中。
因為不適用台灣特色的《特管辦法》,所以《查核基準》把 ISO15189:2012 在章節 4.4.1.f) 下三個註解都槓掉了。
委託檢測
實驗室如有委託需求,須委託符合本指引並經列冊之檢測項目,且實驗室須對受託實驗室檢測結果負責。
| LDTs 查核基準 | ISO 15189:2012,4.5 |
|---|---|
| 4.2 委託檢測 4.2.1 選擇與評估受委託實驗室與諮詢顧問 – 實驗室應有文件化的程序,以評估與選擇有能力的受委託實驗室與提供任何學科其複雜測試之解釋意見的諮詢顧問。 – 此程序應確保符合以下情況: a)實驗室應負責選擇受委託實驗室與受委託諮詢顧問,監控執行的品質並確保受委託實驗室或受委託諮詢顧問有能力執行委託的檢測。當適當時可諮詢實驗室服務使用者意見 。 b)定期審查與評估受委託實驗室與諮詢顧問的協議,以確保符合本查核基準相關條文。 c)定期審查的紀錄,應加以維持。 d)應登錄所有受委託實驗室或尋求意見的諮詢顧問,並予以維持。 e)所有委託檢測的申請與結果,應依事先明訂的期限予以保存。 4.2.2 檢測結果的提供 – 除非協議另有規定,委託實驗室(非指受委託實驗室)應負責受委託實驗室提供給申請者的檢測結果。 – 若由委託實驗室負責發檢測結果單,則檢測結果單中應包括受委託實驗室或諮詢顧問結果中之必要要素,不可因修改而影響臨床結果解釋。檢測結果單應指出那項檢測是由受委託實驗室或諮詢顧問執行。 – 提供這些額外評論之說明者應加以清楚地識別。 – 實驗室應採用最適當方式來發放委託實驗室結果,可考量檢測結果單完成時間、量測準確性、轉錄流程及解釋技巧的要求等。 – 假如正確的解釋與檢測結果的應用,需由委託與受委託實驗室的臨床醫師與專家間共同配合,該流程不應受商業或財務考量所妨礙。 | 4.5 Examination by referral laboratories 4.5.1 Selecting and evaluating referral laboratories and consultants The laboratory shall have a documented procedure for selecting and evaluating referral laboratories and consultants who provide opinions as well as interpretation for complex testing in any discipline. The procedure shall ensure that the following conditions are met. a)The laboratory, with the advice of users of laboratory services where appropriate, is responsible for selecting the referral laboratory and referral consultants, monitoring the quality of performance and ensuring that the referral laboratories or referral consultants are competent to perform the requested examinations. b)Arrangements with referral laboratories and consultants are reviewed and evaluated periodically to ensure that the relevant parts of this International Standard are met. c)Records of such periodic reviews are maintained. d)A register of all referral laboratories, and consultants from whom opinions are sought, is maintained. e)Requests and results of all samples referred are kept for a pre-defined period. 4.5.2 Provision of examination results Unless otherwise specified in the agreement, the referring laboratory(and not the referral laboratory)shall be responsible for ensuring that examination results of the referral laboratory are provided to the person making the request. When the referring laboratory prepares the report, it shall include all essential elements of the results reported by the referral laboratory or consultant, without alterations that could affect clinical interpretation. The report shall indicate which examinations were performed by a referral laboratory or consultant. The author of any additional remarks shall be clearly identified. Laboratories shall adopt the most appropriate means of reporting referral laboratory results, taking into account turnaround times, measurement accuracy, transcription processes and interpretative skill requirements. In cases where the correct interpretation and application of examination results needs collaboration between clinicians and specialists from both referring and referral laboratories, this process shall not be hindered by commercial or financial considerations. |
建議符合方式:
如果所提供的檢測服務不需要委外,檢測前、中、後(例如:解讀報告)也不需要聘請專家(例如:病理科醫師),這項就可以排除。
有委外檢測的需求時,建議先與食藥署承辦人確認是否可以委外,因為關鍵流程不可委外(請見下方食藥署 FQA)。但有什麼是關鍵流程呢?請先去找食藥署討論,避免送件後才被打槍,重新規劃流程、確效可是曠日廢時的呢!
28. 申請食藥署 LDTs 認證,能否將部分檢測流程委託外部實驗室辦理?
說明:實驗室申請 LDTs 認證,應具備必要檢測儀器、設備及場地,能自行執行檢測,關鍵步驟不得委外原則。如有部分流程委外,受委託者須符合精準醫療分子檢測實驗室檢測與服務指引並經品質認證之實驗室,且實驗室應對受託實驗室檢測結果負責。
– 《精準醫療分子檢測實驗室認證》第 28 題問答(另請參考第 15 題問答)
外部的服務與供應
實驗室需對外來服務及供應項目之選擇進行評估,並有適切標示要求,進行監控,以確保相關品質以確保檢測之結果不受影響。
| LDTs 查核基準 | ISO 15189:2012,4.6 |
|---|---|
| 4.3 外部的服務與供應 – 實驗室應有文件化的程序,以選擇與採購可影響其服務品質之外部服務、設備、試劑及耗材(同時參見 1.6)。 – 基於供應外部服務、設備、試劑及耗材之能力,實驗室應選擇與審查符合實驗室要求的供應商。惟可視需求,與機構內其他部門或相關職務人員合作,以達成該要求。選擇的準則應予以建立。 – 經評選認可的設備、試劑及耗材供應商之清單,應予以維持。 – 採購資訊應說明擬採購產品或服務的要求。 – 實驗室應監控供應商服務表現,以確保採購服務或項目持續符合所聲明的準則。 | 4.6 External services and supplies The laboratory shall have a documented procedure for the selection and purchasing of external services, equipment, reagents and consumable supplies that affect the quality of its service(see also 5.3). The laboratory shall select and approve suppliers based on their ability to supply external services, equipment, reagents and consumable supplies in accordance with the laboratory’s requirements; however, it may be necessary to collaborate with other organizational departments or functions to fulfil this requirement. Criteria for selection shall be established. A list of selected and approved suppliers of equipment, reagents and consumables shall be maintained. Purchasing information shall describe the requirements for the product or service to be purchased. The laboratory shall monitor the performance of suppliers to ensure that purchased services or items consistently meet the stated criteria. |
建議符合方式:
可以把這部分的規定詳細規範在《供應商及採購管理程序》中。
諮詢服務
實驗室應確保與醫療機構溝通之管道與程序,以確保其檢測與服務之品質(包含檢測規格釐清與訂定、檢測結果之呈現說明等)。
| LDTs 查核基準 | ISO 15189:2012,4.7 |
|---|---|
| 4.4 諮詢服務 – 實驗室應建立下列與使用者溝通的安排: a)檢測的選擇與服務的使用,包括所需求的樣本種類(同時參見 5.1)、適應症與檢測程序限制及檢測申請的頻率等諮詢; b)檢測技術諮詢; d)促進實驗室服務的有效運用; e)科學與邏輯事宜的諮詢,例如樣本未符合接受準則的案例。 | 4.7 Advisory services The laboratory shall establish arrangements for communicating with users on the following: a)advising on choice of examinations and use of the services, including required type of sample(see also 5.4), clinical indications and limitations of examination procedures and the frequency of requesting the examination; b)advising on individual clinical cases; d)promoting the effective utilization of laboratory services; e)consulting on scientific and logistic matters such as instances of failure of sample(s) to meet acceptance criteria. |
建議符合方式:
我習慣盡可能地精簡文件,所以會把所有對外溝通的方式都用《客訴與回饋管理程序》管理,因此,諮詢服務的詳細規定也可以寫在這本二階程序書中。不過,因為諮詢內容涉及專業知識,最好也把諮詢人員的資格、考核方式規定在《教育訓練與員工資格管理程序》。
抱怨的解決
實驗室應有作業標準與標準作業程序,管理來自於醫療機構的抱怨或各項回饋。
| LDTs 查核基準 | ISO 15189:2012,4.8 |
|---|---|
| 4.5 抱怨的解決 – 實驗室應有文件化的程序,以管理來自於申請者、實驗室員工或其他當事人的抱怨或各 項回饋。所有抱怨與其調查紀錄及採行之措施, 應予以維持(同時見 3.5.3)。 | 4.8 Resolution of complaints The laboratory shall have a documented procedure for the management of complaints or other feedback received from clinicians, patients, laboratory staff or other parties. Records shall be maintained of all complaints and their investigation and the action taken(see also 4.14.3). |
建議符合方式:
就用《客訴與回饋管理程序》來結束這一回合吧。

8.5 技術要求
檢測前流程
實驗室於檢體接收、運送及儲存等程序應有標準化流程並文件化,並提供相關資訊給醫療機構。
| LDTs 查核基準 | ISO 15189:2012,5.4 |
|---|---|
| 5.1 檢測前流程 5.1.1 概述 – 針對檢測前作業活動,實驗室應有文件化的程序與資訊,以確保檢測結果的有效性。 5.1.2 提供與使用者的資訊 – 實驗室應有資訊提供實驗室服務的與使用者取用。 – 此資訊應適當的包含: a)實驗室的地點; b)實驗室提供的服務形式,包括委託其他實驗室的檢測; c)實驗室的服務時間; d)實驗室所提供的檢測,適當的包括,所需樣本相關資訊、原始樣本體積、特別注意事項、檢測結果單完成時間(可能以一般檢測類別或檢測群組方式提供); e)生物參考區間; f)完成檢測申請單的說明; i)運送樣本的說明,包括任何特殊必要處理; k)實驗室接受與拒收樣本的準則; l)顯著影響檢測性能或結果解釋的已知因素清單; n)實驗室保護個人資訊的政策; o)抱怨實驗室的程序。 5.1.3 檢測申請單資訊 – 檢測申請單或功能相當的電子式申請,其欄位應包括以下,但不限: a)檢體的唯一識別; 附註:唯一識別包括字母及/或數字的識別。 b)臨床醫師、健康照護提供者、或其他申請檢測或使用醫療資訊的法定授權人士的姓名或唯一識別,與連同檢測結果單收件目的地與連絡人資料; c)原始樣本的類型,與當相關時,檢體來源的解剖位置; d)申請的檢測項目; f)原始樣本採檢的日期,當相關時,與時間; g)樣本接收的日期與時間。 附註: – 檢測申請單之格式(例如,電子或紙本式)與申請方式,實驗室須與服務使用者溝通討論決定。 – 關於口頭檢測申請,實驗室應有文件化的程序,包括以檢測申請單或功能相當的電子式申請,在約定時間內加以確認。(可否允許口頭檢測申請)實驗室應願意與使用者或其代表合作,以釐清使用者的申請。 | 5.4 Pre-examination processes 5.4.1 General The laboratory shall have documented procedures and information for pre-examination activities to ensure the validity of the results of examinations. 5.4.2 Information for The laboratory shall have information available for a)the location of the laboratory; b)types of clinical services offered by the laboratory including examinations referred to other laboratories; c)opening hours of the laboratory; d)the examinations offered by the laboratory including, as appropriate, information concerning samples required, primary sample volumes, special precautions, turnaround time,(which may also be provided in general categories or for groups of examinations), biological reference intervals e)instructions for completion of the request form; g)instructions for patient-collected samples; h)instructions for transportation of samples, including any special handling needs; j)the laboratory’s criteria for accepting and rejecting samples; k)a list of factors known to significantly affect the performance of the examination or the interpretation of the results; m)the laboratory’s policy on protection of personal information; n)the laboratory’s complaint procedure. 5.4.3 Request form information The request form or an electronic equivalent shall allow space for the inclusion of, but not be limited to, the following: a) NOTE Unique identification includes an alpha and/or numerical identifier b)name or other unique identifier of clinician, healthcare provider, or other person legally authorized to request examinations or use medical information, together with the destination for the report and contact details; c)type of primary sample and, where relevant, the anatomic site of origin; d)examinations requested; NOTE Information needed for examination performance and results interpretation may include the patient’s ancestry, family history, travel and exposure history, communicable diseases and other clinically relevant information. Financial information for billing purposes, financial audit, resource management and utilization reviews may also be collected. The patient should be aware of the information collected and the purpose for which it is collected. f)date and, where relevant, time of primary sample collection; g)date and time of sample receipt. NOTE The format of the request form(e.g. electronic or paper)and the manner in which requests are to be communicated to the laboratory should be determined in discussion with the users of laboratory services. The laboratory shall have a documented procedure concerning verbal requests for examinations that includes providing confirmation by request form or electronic equivalent within a given time. The laboratory shall be willing to cooperate with users or their representatives in clarifying the user’s request. |
建議符合方式:
將檢測前作業活動的規定明訂於《檢體接收與處理管理程序》,並且可寫一份《XX 服務須知》或者《XX 採檢手冊》,將「5.1.2 提供與使用者的資訊」的內容寫在裡面,必要時可提供給合作的醫療機構。
「5.1.3 檢測申請單資訊」規定要有一個《檢測申請單》,在未來認證流程中,這個表單內容會被「多次」要求修改。(是的,不會一次說完要改啥,可能會分成很多次,並在不同階段,由不同審查者給予不同的意見 (◞‸◟))
| LDTs 查核基準 | ISO 15189:2012,5.4 |
|---|---|
| 5.1.4 原始樣本的處理 5.1.4.1 概述 – 實驗室應有文件化的程序,做為原始樣本的標準程序,必要時此文件化程序應提供給委託者使用。 – 當使用者的要求與文件化採檢程序有所差異(排除)或附加,這些內容應予以記錄與納入有包含該檢測結果的所有文件,並應與適當人員溝通。 | 5.4.4 Primary sample collection and handling 5.4.4.1 General The laboratory shall have documented procedures for the proper collection and handling of primary samples. The documented procedures shall be available to those responsible for primary sample collection Where the user requires deviations and exclusions from, or additions to, the documented collection procedure, these shall be recorded and included in all documents containing examination results and shall be communicated to the appropriate personnel. Special procedures, including more invasive procedures, or those with an increased risk of complications to the procedure, will need a more detailed explanation and, in some cases, written consent. In emergency situations, consent might not be possible; under these circumstances it is acceptable to carry out necessary procedures, provided they are in the patient’s best interest. NOTE 2 Adequate privacy during reception and sampling should be available and appropriate to the type of information being requested and primary sample being collected. 5.4.4.2 Instructions for pre-collection activities The laboratory’s instructions for pre-collection activities shall include the following: a)completion of request form or electronic request; b)preparation of the patient(e.g. instructions to caregivers, phlebotomists, sample collectors and patients); c)type and amount of the primary sample to be collected with descriptions of the primary sample containers and any necessary additives; d)special timing of collection, where needed; e)clinical information relevant to or affecting sample collection, examination performance or result interpretation(e.g. history of administration of drugs). 5.4.4.3 Instructions for collection activities The laboratory’s instructions for collection activities shall include the following: a)determination of the identity of the patient from whom a primary sample is collected; b)verification that the patient meets pre-examination requirements [e.g. fasting status, medication status (time of last dose, cessation), sample collection at predetermined time or time intervals, etc.]; c)instructions for collection of primary blood and non-blood samples, with descriptions of the primary sample containers and any necessary additives; d)in situations where the primary sample is collected as part of clinical practice, information and instructions regarding primary sample containers, any necessary additives and any necessary processing and sample transport conditions shall be determined and communicated to the appropriate clinical staff; e)instructions for labelling of primary samples in a manner that provides an unequivocal link with the patients from whom they are collected; f)recording of the identity of the person collecting the primary sample and the collection date, and, when needed, recording of the collection time; g)instructions for proper storage conditions before collected samples are delivered to the laboratory; h)safe disposal of materials used in the collection. |
建議符合方式:
《檢體接收與處理管理程序》內要明訂原始檢體的標準處理程序;另外可創建《檢測及報告產出管理程序》,說明如果實際的採檢程序與標準程序不同時,應該如何記錄、如何納入檢測報告中。
還有,所有不符合事件的處置、記錄相關規定都可以引用《不符合事件管理程序》,這邊採檢程序的差異(可當作一種不符合事件)也不例外,可在《不符合事件管理程序》中規定應該如何記錄、溝通。
ISO 15189:2015 這部分有很大一段都沒被食藥署引用至《查核基準》,因為那部分是關於醫療機構對病人、受試者,或者醫療機構運檢體到實驗室的規定,但在台灣特色的規範中,業界的「特定實驗室」並不能直接和病人、受試者接觸(請參考「LDTs 管理架構概述圖」),因此《查核基準》槓掉此段。
(在《查核基準》5.1.4.1 章節規定:「實驗室應有文件化的程序,做為原始樣本的標準程序…,」但是,是原始樣本的什麼規定?《查核基準》中沒寫出來,看了原文才知道是關於原始樣本的 proper collection and handling 規定 ¯_(ツ)_/¯)
| LDTs 查核基準 | ISO 15189:2012,5.4 |
|---|---|
| 5.1.5 樣本運送 – 採檢後作業活動的實驗室說明應包括樣本運送的包裝。 – 實驗室應有監控運送樣本的文件化程序,以確保: a)在適用於申請檢測的本質與實驗室學科考量的時間範圍內。 b)在原始樣本採檢與處理的特定溫度範圍內及使用指定的保存劑,以確保樣本的完整性。 c)以能確保樣本完整性與運送者、一般公眾及接收實驗室安全的方式運送,且應符合已建立的要求。 附註:實驗室雖未涉及原始樣本的採檢與運送,當接收到完整性遭質疑,或其可能危害運送者或一般公眾安全的樣本時,具立即聯繫寄送人並告知採取的步驟以避免再發生,亦被視為已滿足上述 5.1.5 c)條文 | 5.4.5 Sample transportation The laboratory’s instructions for post-collection activities shall include packaging of samples for transportation. The laboratory shall have a documented procedure for monitoring the transportations of samples to ensure they are transported: a)within a time frame appropriate to the nature of the requested examinations and the laboratory discipline concerned; b)within a temperature interval specified for sample collection and handling and with the designated preservatives to ensure the integrity of samples; c)in a manner that ensures the integrity of the sample and the safety for the carrier, the general public and the receiving laboratory, in compliance with established requirements. NOTE A laboratory which is not involved in primary sample collection and transportation is considered to have satisfied clause 5.4.5 c) above when, upon receipt of a sample whose integrity was compromised or which could have jeopardized the safety of the carrier or the general public, the sender is contacted immediately and informed about measures to be taken to eliminate recurrence. |
建議符合方式:
《檢體接收與處理管理程序》裡面可以將這部分的要求明文規定出來。關於「樣本運送的包裝」可寫在《XX 服務須知》或者《XX 採檢手冊》中。
| LDTs 查核基準 | ISO 15189:2012,5.4 |
|---|---|
| 5.1.6 樣本接收 – 實驗室的樣本接收程序,應確保符合下列條件: a)以檢測申請或標示,樣本可明確追溯到已識別的或其位置。(但不得有受檢者姓名、身分證字號等足以辨識個人之資料) b)實驗室自訂並文件化的接收或拒絕樣本準則,予以實施。 c)當樣本由於延誤運送或不當容器造成樣本的不穩定、樣本容積不足,或當樣本有臨床緊急的或不可替代時,而實驗室選擇處理樣本,最終檢測結果單應顯示問題本質。當適合時,應小心謹慎解釋結果。 d)所有已接收的樣本記錄於登記本、工作單、電腦或其他相當的系統中。樣本接收/或登記的日期與時間應予以記錄。當可能時,樣本接收人員的識別,應予以記錄。 e)被授權的人員應評估所接收的樣本,以確保符合相關申請檢測項目的接受準則。 f)當相關時,對特別標註為緊急的樣本,其接收、標示、處理及檢測結果單應予以說明。此說明應包括檢測申請單與樣本的任何特別標示細節、樣本至實驗室檢測區的運送機制、任何快速處理模式的使用,以及任何遵循的特別發放檢測結果單之準則。 – 所有原始樣本的分裝,應能明確地追溯至最初原始樣本。 | 5.4.6 Sample reception The laboratory’s procedure for sample reception shall ensure that the following conditions are met. a)Samples are unequivocally traceable, by request and labelling, to an identified patient or site. b)Laboratory-developed and documented criteria for acceptance or rejection of samples are applied. c)Where there are problems with d)All samples received are recorded in an accession book, worksheet, computer or other comparable system. The date and time of receipt and e)Authorized personnel shall evaluate received samples to ensure that they meet the acceptance criteria relevant for the requested examination(s). f)Where relevant, there shall be instructions for the receipt, labelling, processing and reporting of samples specifically marked as urgent. The instructions shall include details of any special labelling of the request form and sample, the mechanism of transfer of the sample to the examination area of the laboratory, any rapid processing mode to be used, and any special reporting criteria to be followed. All portions of the primary sample shall be unequivocally traceable to the original primary sample. |
建議符合方式:
這部分的規定也可以寫在《檢體接收與處理管理程序》。但《特管辦法》規定業界實驗室(特定實驗室)不可和受檢者接觸(請參考「LDTs 管理架構概述圖」),因此,在《LDTs 查核基準》5.1.6.a) 中規定,檢測申請單中不可有受檢者姓名、身分證字號等足以辨識個人之資料。
| LDTs 查核基準 | ISO 15189:2012,5.4 |
|---|---|
| 5.1.7 檢測前處理、準備及儲存 – 實驗室應有程序與適當設施,於檢測前作業活動與處理、準備及儲存過程中,保護樣本與避免其變質、遺失或損壞。 – 實驗室程序應包括於同一原始樣本,申請附加檢測或進一步檢測的時間限制。 | 5.4.7 Pre-examination handling, preparation and storage The laboratory shall have procedures and appropriate facilities for securing patient samples and avoiding deterioration, loss or damage during pre-examination activities and during handling, preparation and storage. Laboratory procedures shall include time limits for requesting additional examinations or further examinations on the same primary sample. |
建議符合方式:
一樣用《檢體接收與處理管理程序》結束這回合。
檢測流程
檢測程序應經確效,並文件化。
| LDTs 查核基準 | ISO 15189:2012,5.5 |
|---|---|
| 5.2 檢測流程 5.2.1 檢測程序的選擇、查證及確認 5.2.1.1 概述 – 實驗室應選擇已經確認符合使用意圖的檢測程序。執行檢測流程作業活動的人員身份應予以記錄。 – 每項檢測程序的特定要求(性能規格),應與該檢測項目的使用意圖相關。 附註:首選程序為那些已規定於體外醫療器材的使用說明書,或那些已發佈在已建立或權威教科書、同儕審查的教科書文章或期刊,或在國際共識的標準或指引,或國家或區域的法規中。 5.2.1.2 檢測程序的查證 – 使用已確認且未經修改的檢測程序,於導入例行檢測使用前應經過實驗室獨立查證。 – 實驗室應取得來自於製造商/方法開發者的資訊,以證實程序的性能特徵。- 由實驗室的獨立查證,應透過取得客觀證據(以性能特徵(performance characteristics)的型式),以證實已符合檢測程序所宣告的性能。 – 查證流程中所證實的檢測程序之宣告性能,應與檢測結果的使用意圖相關。 – 實驗室應將所使用的查證程序文件化並記錄其所取得結果。具適當權責的人員應審查查證的結果並記錄此審查。 | 5.5 Examination processes 5.5.1 Selection, verification and validation of examination procedures 5.5.1.1 General The laboratory shall select examination procedures which have been validated for their intended use. The identity of persons performing activities in examination processes shall be recorded. The specified requirements(performance specifications)for each examination procedure shall relate to the intended use of that examination. NOTE Preferred procedures are those specified in the instructions for use of in vitro medical devices or those that have been published in established/authoritative textbooks, peer-reviewed texts or journals, or in international consensus standards or guidelines, or national or regional regulations. 5.5.1.2 Verification of examination procedures Validated examination procedures used without modification shall be subject to independent verification by the laboratory before being introduced into routine use. The laboratory shall obtain information from the manufacturer/method developer for confirming the performance characteristics of the procedure. The independent verification by the laboratory shall confirm, through obtaining objective evidence(in the form of performance characteristics)that the performance claims for the examination procedure have been met. The performance claims for the examination procedure confirmed during the verification process shall be those relevant to the intended use of the examination results. The laboratory shall document the procedure used for the verification and record the results obtained. Staff with the appropriate authority shall review the verification results and record the review. |
建議符合方式:
將「選擇已經確認符合使用意圖的檢測程序」相關規定制訂於《檢體接收與處理管理程序》,另外在《開發、查證及確效管理程序》裡面制訂檢測技術查證的規定。
估狗或在食藥官網搜尋後,可以找到《精準醫療分子檢測實驗室檢測技術指引 – 次世代定序應用於腫瘤檢測(草案)》和《精準醫療分子檢測實驗室檢測技術指引 – 次世代定序應用於遺傳類疾病檢測》。
在食藥署官網的「法規資訊 > 檢驗類」中還可以看到《精準醫療分子檢測實驗室檢測技術指引-次世代定序應用於遺傳類疾病檢測》,但點開連結後只顯示「前並無相關資料」,而且找不到《精準醫療分子檢測實驗室檢測技術指引 – 次世代定序應用於腫瘤檢測(草案)》。
這個食藥署官網齁 ʅ(´◔౪◔)ʃ
| LDTs 查核基準 | ISO 15189:2012,5.5 |
|---|---|
| 5.2.1.3 檢測程序的確認 – 實驗室應確認下列來源的檢測程序: a)非標準方法; b)實驗室自行設計或開發的方法; c)標準方法但使用於預期範圍以外; d)已確認方法但經修訂過。 – 確認作業應依需要盡可能的廣泛,並透過客觀證據的提供(以性能特徵的型式),證實符合檢測使用意圖的特定要求。 附註:一個檢測程序的性能特徵,須考量包括到:量測真實度、量測準確度、量測精密度包括量測重複性與量測中間精密度;量測不確定度、特異性,包括干擾物質、敏感度、偵測極限與定量極限、量測區間。 – 實驗室應將所使用的確認程序文件化,並記錄其所取得結果。具適當權責的人員應審查確認的結果並記錄此審查。 – 當已確認的檢測程序有改變時,該改變的影響應予以文件化,適當時,新的確認作業應予以實施。 5.2.1.4 定量量測值的量測不確定度 – 實驗室應決定在檢測階段的每項量測程序其用於呈現樣本的定量量測值之量測不確定度。 – 實驗室應明訂每項量測程序其量測不確定度的性能要求,並定期審查量測不確定度的估計值。 附註 1:相關不確定度組成與實際量測流程有關,開始於樣本提交予量測程序與量測數據的產出為止。 附註 2:量測不確定度,可在中間精密度(Intermediate Precision)條件下,採取量測品管物質的量值,計算得出。此條件包括在量測程序標準作業中合理可能的許多常規改變,例如,試劑與校正批號的改變、不同操作人員、定期儀器保養等。 附註 3:量測不確定度估計的實際應用,舉例可能包括確認檢測值符合實驗室設定的品質目標(quality goals),與檢測值跟先前相同類型的檢測值,或其與臨床決策值進行有意義的比對。 – 當實驗室解釋量測的量值時,應考慮量測不確定度。當有要求時,實驗室應為實驗室使用者提供其量測不確定度估計值。 – 當檢測包括一個不用呈現量測量值的量測步驟時,而該步驟有助於評鑑檢測可信度或影響檢測結果,實驗室須計算此量測步驟的不確定度。 | 5.5.1.3 Validation of examination procedures The laboratory shall validate examination procedures derived from the following sources: a)non-standard methods; b)laboratory designed or developed methods; c)standard methods used outside their intended scope; d)validated methods subsequently modified. The validation shall be as extensive as is necessary and confirm, through the provision of objective evidence(in the form of performance characteristics), that the specific requirements for the intended use of the examination have been fulfilled. NOTE Performance characteristics of an examination procedure should include consideration of: measurement trueness, measurement accuracy, measurement precision including measurement repeatability and measurement intermediate precision; measurement uncertainty, The laboratory shall document the procedure used for the validation and record the results obtained. Staff with the authority shall review the validation results and record the review. When changes are made to a validated examination procedure, the influence of such changes shall be documented and, when appropriate, a new validation shall be carried out. 5.5.1.4 Measurement uncertainty of measured quantity values The laboratory shall determine measurement uncertainty for each measurement procedure in the examination phase used to report measured quantity values on patients’ samples. The laboratory shall define the performance requirements for the measurement uncertainty of each measurement procedure and regularly review estimates of measurement uncertainty. NOTE 1 The relevant uncertainty components are those associated with the actual measurement process, commencing with the presentation of the sample to the measurement procedure and ending with the output of the measured value. NOTE 2 Measurement uncertainties may be calculated using quantity values obtained by the measurement of quality control materials under intermediate precision conditions that include as many routine changes as reasonably possible in the standard operation of a measurement procedure, e.g. changes of reagent and calibrator batches, different operators, scheduled instrument maintenance. NOTE 3 Examples of the practical utility of measurement uncertainty estimates might include confirmation that patients’ values meet quality goals set by the laboratory and meaningful comparison of a patient value with a previous value of the same type or with a clinical decision value. The laboratory shall consider measurement uncertainty when interpreting measured quantity values. Upon request, the laboratory shall make its estimates of measurement uncertainty available to laboratory users. Where examinations include a measurement step but do not report a measured quantity value, the laboratory should calculate the uncertainty of the measurement step where it has utility in assessing the reliability of the examination procedure or has influence on the reported result. |
建議符合方式:
《開發、查證及確效管理程序》可用來規範「檢測程序的確認」細節;《變更管理程序》則可用來確保「檢測程序有改變時」,如何記錄與評估相關資訊、影響。
另外,可將「定量量測值的量測不確定度」的規定制訂於《量測不確定度及生物參考區間管理程序》。
何時要計算量測不確定度呢?ISO 15189:2012 原文比較清楚:
The laboratory shall determine measurement uncertainty for each measurement procedure in the examination phase used to report measured quantity values on patients’ samples.
Where examinations include a measurement step but do not report a measured quantity value, the laboratory should calculate the uncertainty of the measurement step where it has utility in assessing the reliability of the examination procedure or has influence on the reported result.
– ISO 15189:2012, 5.5.1.4 Measurement uncertainty of measured quantity values
因此,只有當最終報告上呈現的是檢體的定量量測數值,才必須要決定量測不確定度。
換句話說,最終報告上不是呈現檢體的定量量測值,就一定不用計算量測不確定度嗎?
不一定。只要檢測過程中有定量量測值,且當量測不確定度「有助於評鑑檢測可信度或影響檢測結果」時,就還是要計算量測不確定度。
請參考 TAF 提供的參考指引:《醫學實驗室定量量測不確定度評估案例》&《以定性呈現最終結果報告之定量測試的量測不確定度評估案例》來建立自己的量測不確定度。
因為要「定期審查量測不確定度的估計值」,所以可以在《管理審查管理程序》裡面增加這項審查項目,這樣就不會忘記了。
有些公司的變更管制表單中只有一堆空白欄位讓簽核的人各自發揮,而我覺得比較好的做法是把官方的變更審查規定放進變更管制表單中,讓簽核的人可以有個審查依據。醫療器材方面可參考的指引很多,例如《上市後醫材設計 (工程) 變更會影響到許可證?關於美國 FDA、台灣食藥署 TFDA 的規定,本筆記整理給你!》一文中引用的參考指引。不過,《特管辦法》目前只有《各項變更申請送審資料對照表(附件二)》可以看了。
| LDTs 查核基準 | ISO 15189:2012,5.5 |
|---|---|
| 5.2.2 生物參考區間或閾值 – 實驗室必要時應明訂生物參考區間或閾值,將參考區間或閾值依據予以文件化並與使用者溝通此資訊。 當某一特定生物參考區間或閾值與所服務族群不再有相關時,應採取適度改變並與使用者溝通。 – 當實驗室改變檢測程序或檢測前程序,實驗室應審查有關的參考區間與閾值,當適用時。 5.2.3 檢測程序的文件化 – 檢測程序應予文件化。它們應使用實驗室人員普遍瞭解的語言編寫,並放在容易取得的適當地點。 – 任何精簡的文件形式(例如,卡片檔案或類似應用系統),應與已文件化的程序相符合。 附註 1:在有完整的文件化程序可供參考下,可接受於工作檯面有摘要關鍵資訊的工作說明、卡片檔案或類似系統,用於快速參考。 附註 2:使用來自產品說明的資訊,可以參考文件的方式納入檢測程序。 – 與執行檢測有關的所有文件,包括程序、摘要文件、精簡文件形式及產品使用說明等,應納入文件管制。 – 除文件管制識別外,當適用於檢測程序時,文件應包括以下: a)檢測的目的; b)檢測所使用程序的原理與方法; c)性能特徵(見 5.2.1.2 及 5.2.1.3); d)樣本的種類(例如,血漿、血清,尿液); e)容器與添加劑的種類; f)所需的設備與試劑; g)環境與安全管制; h)校正程序(量測追溯); i)程序步驟; j)品質管制程序; k)干擾(例如,脂血、溶血、膽紅素血症、藥物等)與交互反應; l)計算結果程序的原理,包括相關時,量測量值的量測不確定度; m)生物參考區間或閾值; n)檢測結果的可報告區間或閾值; o)當結果不在量測區間內時,決定定量結果的說明; p)警告/危急值,當適當時; r)變異的潛在來源; s)參考文件; t)樣本接收標準及後續不良樣本處理之標準作業程序。 – 如果實驗室打算改變現有檢測程序,以致其結果或結果解釋可能有顯著差異時,該程序經確認後,應向實驗室服務的使用者解釋其影響。 附註 3:此要求可視當地情況,以各種方式達成。有些方法包括直接郵寄、實驗室時事通訊(newsletters)、或為檢測結果單本身的一部份。 | 5.5.2 Biological reference intervals or clinical decision values The laboratory shall define the biological reference intervals or clinical decision values, document the basis for the reference intervals or decision values and communicate this information to users. When a particular biological reference interval or decision value is no longer relevant for the population served, appropriate changes shall be made and communicated to the users. When the laboratory changes an examination procedure or pre-examination procedure, the laboratory shall review associated reference intervals and clinical decision values, as applicable. 5.5.3 Documentation of examination procedures Examination procedures shall be documented. They shall be written in a language commonly understood by the staff in the laboratory and be available in appropriate locations. Any condensed document format(e.g. card files or similarly used systems)shall correspond to the documented procedure. NOTE 1 Working instructions, card files or similar systems that summarize key information are acceptable for use as a quick reference at the workbench, provided that a full documented procedure is available for reference. NOTE 2 Information from product instructions for use may be incorporated into examination procedures by reference. All documents that are associated with the performance of examinations, including procedures, summary documents, condensed document format and product instructions for use, shall be subject to document control. In addition to document control identifiers, documentation shall include, when applicable to the examination procedure, the following: a)purpose of the examination; b)principle and method of the procedure used for examinations; c)performance characteristics(see 5.5.1.2 and 5.5.1.3); d)type of sample(e.g. plasma, serum, urine); f)type of container and additives; g)required equipment and reagents; h)environmental and safety controls; i)calibration procedures(metrological traceability); j)procedural steps; k)quality control procedures; l)interferences(e.g. lipaemia, haemolysis, bilirubinemia, drugs)and cross reactions; m)principle of procedure for calculating results including, where relevant, the measurement uncertainty of measured quantity values; n)biological reference intervals or clinical decision values; o)reportable interval of examination results; p)instructions for determining quantitative results when a result is not within the measurement interval; q)alert/critical values, where appropriate; s)potential sources of variation; t)references. If the laboratory intends to change an existing examination procedure such that results or their interpretations could be significantly different, the implications shall be explained to users of the laboratory services after validating the procedure. NOTE 3 This requirement can be accomplished in different ways, depending on local circumstances. Some methods include directed mailings, laboratory newsletters or part of the examination report itself. |
建議符合方式:
《量測不確定度及生物參考區間管理程序》可用來制訂生物參考區間,並用《變更管理程序》來保障所有變更都不會影響原本已建立的流程、已發的報告的有效性。
「檢測程序的文件化」的相關規定可制訂於《檢測及報告產出管理程序》及《文件與紀錄管理程序》。
要特別注意的是,「摘要文件、精簡文件形式」也必須納入文件管制。所以,至少實地查核前,要清掉所有實驗人員自己的筆記!
另外,《LDTs 查核基準》沒有類似美國 FDA 在 Sec. 820.181 Device master record(DMR)規定,也沒有 Sec. 820.30 Design controls 的規定,所以如果不知道要在哪裡把 LDTs 各項規格定義清楚的話,可以為每個 LDT 建立一個總的 SOP,將《LDTs 查核基準》「5.2.3 檢測程序的文件化」第 a) 到 t) 都寫進去,把這本總 SOP 當作 DMR。
DMR 就像是一項產品的「粽子頭」,只要拿出 DMR,就可以直接看到,或索引到產品所有重要資訊。
曾經聽過一個說法,「想像你在一家製造對全人類極度重要醫療器材的公司,而且地球上就只有你這家公司有辦法製造這個產品。有天,你們公司全員去搭郵輪員工旅遊,結果船沉了,人也全沒了。政府為了全人類的生命存續而派人接管你的公司。政府這時候第一件事應該就是找出 MDR。理論上,只要照著這份 DMR,應該就可以製造出一樣安全、有相同功效的產品。」
這就是 DMR 的目的,在 ISO 13485:2016「4.2.3 Medical device file」也有類似的規定。
檢測結果品質的管制
應有檢測結果的品質管制並文件化;另實驗室應參與實驗室間平行比對方案,確保實驗結果之正確性。
| LDTs 查核基準 | ISO 15189:2012,5.6 |
|---|---|
| 5.3 確保檢測結果的品質 5.3.1 概述 – 實驗室應依明訂的條件執行檢測,以確保檢測的品質。 – 適當的檢測前與檢測後的流程應予以實施(見 3.5.7、 5.1、 5.4 及 5.5)。 – 實驗室不得偽造任何結果。 5.3.2 品質管制 5.3.2.1 概述 – 實驗室應設計品質管制程序,以查證其結果達到預期的品質。 附註:在若干國家,品質管制,如同本次條款所提及,亦稱為「內部品質管制」。 5.3.2.2 品管物質 – 實驗室應使用品管物質,其在檢測系統反應中儘可能接近樣本型式。 – 應定期使用品管物質執行檢測,其頻率是基於程序的穩定度與錯誤結果傷及的風險為基礎。 附註 1:實驗室須選擇品管物質的濃度,當可能時,特別是在或接近臨床決策值,其可確保決策的有效性。 附註 2:須考量使用獨立第三方品管物質,不論是取代或額外附加在任何由試劑或儀器製造商所供應的品管物質。 5.3.2.3 品管數據 – 實驗室應有程序以避免在品管失效情況下,釋出的結果。 – 當違反品管規則與顯示檢測結果可能包含臨床有意義的錯誤,此結果應予以拒絕並在錯誤條件已改進與規格內的性能已查證後,再次複驗相關樣本。 – 實驗室也應評估從最後一次成功品管事件後已檢測的樣本結果。 – 品管數據應定期審查以偵測檢測性能表現趨勢,其可能顯示出檢測系統的問題,當此趨勢被提及註明,預防措施應予執行並記錄。 附註:流程管制之統計與非統計技術須予以使用,無論任何情況可能用於持續監控檢測系統性能。 | 5.6 Ensuring quality of examination results 5.6.1 General The laboratory shall ensure the quality of examinations by performing them under defined conditions. Appropriate pre and post-examination processes shall be implemented(see 4.14.7, 5.4, 5.7 and 5.8). The laboratory shall not fabricate any results. 5.6.2 Quality control 5.6.2.1 General The laboratory shall design quality control procedures that verify the attainment of the intended quality of results. NOTE In several countries, quality control, as referred to in this subclause, is also named “internal quality control.” 5.6.2.2 Quality control materials The laboratory shall use quality control materials that react to the examining system in a manner as close as possible to patient samples. Quality control materials shall be periodically examined with a frequency that is based on the stability of the procedure and the risk of harm to the patient from an erroneous result. NOTE 1 The laboratory should choose concentrations of control materials, wherever possible, especially at or near clinical decision values, which ensure the validity of decisions made. NOTE 2 Use of independent third party control materials should be considered, either instead of, or in addition to, any control materials supplied by the reagent or instrument manufacturer. 5.6.2.3 Quality control data The laboratory shall have a procedure to prevent the release of patient results in the event of quality control failure. When the quality control rules are violated and indicate that examination results are likely to contain clinically significant errors, the results shall be rejected and relevant patient samples re-examined after the error condition has been corrected and within-specification performance is verified. The laboratory shall also evaluate the results from patient samples that were examined after the last successful quality control event. Quality control data shall be reviewed at regular intervals to detect trends in examination performance that may indicate problems in the examination system. When such trends are noted, preventive actions shall be taken and recorded. NOTE Statistical and non-statistical techniques for process control should be used wherever possible to continuously monitor examination system performance. |
建議符合方式:
用《檢測及報告產出管理程序》確保有明確的檢測條件、步驟與報告審核的流程。
在《持續改進管理程序》及《管理審查管理程序》中規定必須定期統計分析與檢視品管數據,以「偵測檢測性能表現趨勢」。如果發現有潛在檢測系統問題時,則依《不符合事件管理程序》執行並記錄預防措施。
| LDTs 查核基準 | ISO 15189:2012,5.6 |
|---|---|
| 5.3.3 實驗室間比對 5.3.3.1 參與 – 實驗室應參與適合檢測項目與檢測結果解釋的實驗室間比對方案(例如外部品質評鑑方案,或能力試驗方案)。 – 實驗室應監控實驗室間比對方案的結果,當未符合預定的表現準則時,應參與矯正措施的實施。 附註:實驗室須參與本質上符合 ISO/IEC 17043 相關要求的實驗室間比對方案。 – 實驗室應建立參與實驗室間比對的文件化程序,包含明訂參與責任與說明、以及任何與實驗室間比對方案已使用準則所不同的表現準則。 – 實驗室所選擇的實驗室間比對方案,應盡可能地提供臨床上相關的挑戰,包括模擬的檢體與有效查核整個檢測過程。當可能時,包括檢測前與檢測後的流程。 5.3.3.2 替代方案 – 當沒有實驗室間比對方案可利用時,實驗室應發展其他方案與提供作為決定檢測結果的可接受度之客觀證據。當可能,這項機制應利用適當的物質。 附註:該類物質的舉例可包括: – 驗證參考物質; – 先前已檢測的樣本; – 取自細胞或組織貯藏處的物質; – 與其他實驗室的交換樣本; – 用於實驗室間比對方案之日常測試的品管物質。 5.3.3.3 實驗室間比對樣本的分析 – 實驗室應將實驗室間比對樣本納入例行工作流程,儘可能依處理樣本的方式處理。 – 實驗室間比對樣本應交由日常檢測樣本人員執行檢測,並採用用於樣本的相同程序。 – 實驗室不應與其他參與實驗室比對方案者交流樣本數據內容,直到提交數據後。 – 實驗室於提交數據前,不應將實驗室間比對樣本委託確認檢測,儘管在常規下可能會執行樣本的委託確認檢測。 5.3.3.4 實驗室表現的評估 – 實驗室間比對表現應被相關人員審查與討論。 – 當未符合預定的表現準則時(即出現不符合事件),實驗室人員應參與矯正措施的實施與記錄。矯正措施的有效性應予以監控。 – 回覆結果應評估其顯示潛在不符合事件之趨勢,並採取預防措施 。 5.3.4 檢測結果的可比較性 – 應有一套清楚的機制,用以比較已使用的程序、設備及方法,並建立涵蓋臨床適當區間之樣本結果間的可比較性。此適用於相同或不同程序、設備、不同地點或包含上述所有。 附註:當量測結果可量測追溯至相同參考來源之特殊情況時,若校正品是具可替換性(commutable),此結果可被視為具量測的可比較性。 – 當量測系統對於相同量測物(例如,葡萄糖),提供不同量測區間與當檢測方法有改變時,實驗室應就其結果間比較的任何差異通知使用者,並討論實務的影響。 – 實驗室應就比對執行的結果予以文件化、記錄,適當時,迅速採取行動。根據鑑別出的問題或缺失應立即行動,並保留行動的紀錄。 附註:關於法律責任考量的某些種類程序,可能較其他樣本,要求較長的保留期限。樣本的安全棄置,應按照作為廢棄物管理的地方法規或建議予以執行。 | 5.6.3 Interlaboratory comparisons 5.6.3.1 Participation The laboratory shall participate in an interlaboratory comparison programme(s)(such as an external quality assessment programme or proficiency testing programme) appropriate to the examination and interpretations of examination results. The laboratory shall monitor the results of the interlaboratory comparison programme(s) and participate in the implementation of corrective actions when predetermined performance criteria are not fulfilled. NOTE The laboratory should participate in interlaboratory comparison programmes that substantially fulfil the relevant requirements of ISO/IEC 17043. The laboratory shall establish a documented procedure for interlaboratory comparison participation that includes defined responsibilities and instructions for participation, and any performance criteria that differ from the criteria used in the interlaboratory comparison programme.Interlaboratory comparison programme(s) chosen by the laboratory shall, as far as possible, provide clinically relevant challenges that mimic patient samples and have the effect of checking the entire examination process, including pre-examination procedures, and post-examination procedures, where possible. 5.6.3.2 Alternative approaches Whenever an interlaboratory comparison is not available, the laboratory shall develop other approaches and provide objective evidence for determining the acceptability of examination results. Whenever possible, this mechanism shall utilize appropriate materials. NOTE Examples of such materials may include: – certified reference materials; – samples previously examined; – material from cell or tissue repositories; – exchange of samples with other laboratories; – control materials that are tested daily in interlaboratory comparison programmes. 5.6.3.3 Analysis of interlaboratory comparison samples The laboratory shall integrate interlaboratory comparison samples into the routine workflow in a manner that follows, as much as possible, the handling of patient samples. Interlaboratory comparison samples shall be examined by personnel who routinely examine patient samples using the same procedures as those used for patient samples. The laboratory shall not communicate with other participants in the interlaboratory comparison programme about sample data until after the date for submission of the data. The laboratory shall not refer interlaboratory comparison samples for confirmatory examinations before submission of the data, although this would routinely be done with patient samples. 5.6.3.4 Evaluation of laboratory performance The performance in interlaboratory comparisons shall be reviewed and discussed with relevant staff. When predetermined performance criteria are not fulfilled(i.e. nonconformities are present), staff shall participate in the implementation and recording of corrective action. The effectiveness of corrective action shall be monitored. The returned results shall be evaluated for trends that indicate potential nonconformities and preventive action shall be taken. 5.6.4 Comparability of examination results There shall be a defined means of comparing procedures, equipment and methods used and establishing the comparability of results for patient samples throughout the clinically appropriate intervals. This is applicable to the same or different procedures, equipment, different sites, or all of these. NOTE In the particular case of measurement results that are metrologically traceable to the same reference, the results are described as having metrological comparability providing that calibrators are commutable. The laboratory shall notify users of any differences in comparability of results and discuss any implications for clinical practice when measuring systems provide different measurement intervals for the same measurand(e.g. glucose) and when examination methods are changed. The laboratory shall document, record and, as appropriate, expeditiously act upon results from the comparisons performed. Problems or deficiencies identified shall be acted upon and records of actions retained. |
建議符合方式:
把「5.3.3 實驗室間比對」及「5.3.4 檢測結果的可比較性」的規定明訂於《實驗室間比對管理程序》,當發生不符合預定的表現時,依照《不符合事件管理程序》執行、記錄矯正措施。另可用《持續改進管理程序》或《管理審查管理程序》來監控實驗室間比對方案的結果。
食藥署的《精準醫療分子檢測實驗室間比對與替代性評估指引》(Backup)是一定要參考的啦!請注意,必須有無法參與「能力試驗活動」,及無法參加實驗室間比對方案的相關書面評估資料,才可以採用最後手段:實驗室内部盲測。
檢測後流程
實驗室應有檢測結果的審查機制及流程,並應文件化;另對於剩餘檢體儲存、保留及棄置應有相關規劃及設計。
| LDTs 查核基準 | ISO 15189:2012,5.7 |
|---|---|
| 5.4 檢測後流程 5.4.1 結果的審查 – 實驗室應有程序以確保檢測結果釋出前已經授權人員的審查,並根據內部品管評估這些檢測結果,適當時,可採用臨床資訊及先前檢測結果。 – 當作為審查結果的程序涉及檢測結果的自動篩選與發放時,審查準則應予以建立、核准及文件化(參見 5.6.1)。 5.4.2 樣本的儲存、保留及棄置 – 實驗室應有文件化的程序作為樣本的鑑別、收集、保留、索引、取用、儲存、維護及臨床樣本的安全棄置。 – 實驗室應明訂臨床樣本的保留期限。應依據樣本本質、檢測及任何適當的要求,明訂保留時間。 | 5.7 Post-examination processes 5.7.1 Review of results The laboratory shall have procedures to ensure that authorized personnel review the results of examinations before release and evaluate them against internal quality control and, as appropriate, available clinical information and previous examination results. When the procedure for reviewing results involves automatic selection and reporting, review criteria shall be established, approved and documented(see 5.9.1). 5.7.2 Storage, retention and disposal of clinical samples The laboratory shall have a documented procedure for identification, collection, retention, indexing, access, storage, maintenance and safe disposal of clinical samples. The laboratory shall define the length of time clinical samples are to be retained. Retention time shall be defined by the nature of the sample, the examination and any applicable requirements. NOTE Legal liability concerns regarding certain types of procedures(e.g. histology examinations, genetic examinations, paediatric examinations) may require the retention of certain samples for much longer periods than for other samples. Safe disposal of samples shall be carried out in accordance with local regulations or recommendations for waste management. |
建議符合方式:
關於「5.4.1 結果的審查」,就用《檢測及報告產出管理程序》規範;《檢體接收與處理管理程序》則用來符合「5.4.2 樣本的儲存、保留及棄置」規定。
檢測結果的確認
應制定及確認檢測結果欄位,並確認檢測結果的呈現符合醫療機構之要求。
| LDTs 查核基準 | ISO 15189:2012,5.8 |
|---|---|
| 5.5 結果的呈現 5.5.1 概述 – 每項檢測的結果應準確地、清晰地、明確地及依據檢測程序的任何特定說明予以呈現。 – 實驗室應明訂檢測結果單的格式與媒體(例如電子式或紙本)以及從實驗室傳遞的方式。 – 實驗室應有程序,以確保實驗室結果轉錄的正確性。 – 檢測結果單應包括檢測結果解釋的所需的資訊。 – 當一個檢測被延誤時,實驗室應有通知申請者的流程。 5.5.2 檢測結果單欄位- 實驗室應確保下列檢測結果單欄位,可有效傳遞實驗室結果並符合使用者的需求: a)可能影響檢測結果的樣本品質備註; b)關於樣本對於接受/拒收準則適用性方面的備註; c)危急值結果,當適用時; d)結果的解釋性備註,當適用時,其中於最終檢測結果單可包括查證的檢測結果的自動篩選與發放之解釋(參見 5.6.2)。 5.5.3 檢測結果單內容 – 檢測結果單應包括但不限於以下: a)清晰、明確的檢測項目識別,當適當時,包括檢測程序; b)出具檢測結果單實驗室的識別; c)由受委託實驗室執行的所有檢測項目的識別; d)每頁檢測結果單均有檢體的識別與所在地點;(不得有受檢者姓名、身分證字號等足以辨識個人之資料) e)申請人姓名或其他唯一識別與申請人的詳細連絡資料; f)原始樣本採檢日期; g)原始樣本的種類; h)量測程序,當適當時; i)檢測結果以 SI 單位呈現,其單位可追溯至 SI 單位,或其他適用的單位; j)生物參考區間、閾值,當適用時; l)其他備註,例如提醒或解釋性附註(例如,可能影響結果的原始樣本的品質或適當性、來自於受委託實驗室的結果與解釋、使用開發中的程序); m)作為研究或發展方案一部份檢測的識別,且無法取得其量測性能的特定宣告; n)審查結果與授權發送檢測結果單人員的識別(若檢測結果單內未包含,可於必要時隨時提供); o)發放的日期,及發送的時間 (若檢測結果單內未包含,可於必要時可隨時提供); p)頁碼與總頁數(例如,「5 頁之 1」,「5 頁之 2」等 )。 | 5.8 Reporting of results 5.8.1 General The results of each examination shall be reported accurately, clearly, unambiguously and in accordance with any specific instructions in the examination procedures. The laboratory shall define the format and medium of the report(i.e. electronic or paper) and the manner in which it is to be communicated from the laboratory. The laboratory shall have a procedure to ensure the correctness of transcription of laboratory results. Reports shall include the information necessary for the interpretation of the examination results. The laboratory shall have a process for notifying the requester when an examination is delayed that could compromise patient care. 5.8.2 Report attributes The laboratory shall ensure that the following report attributes effectively communicate laboratory results and meet the users’ needs: a)comments on sample quality that might compromise examination results; b)comments regarding sample suitability with respect to acceptance/rejection criteria; c)critical results, where applicable; d)interpretive comments on results, where applicable, which may include the verification of the interpretation of automatically selected and reported results(see 5.9.1) in the final report. 5.8.3 Report content The report shall include, but not be limited to, the following: a)a clear, unambiguous identification of the examination including, where appropriate, the examination procedure; b)the identification of the laboratory that issued the report; c)identification of all examinations that have been performed by a referral laboratory; d)patient identification and patient location on each page; e)name or other unique identifier of the requester and the requester’s contact details; f)date of primary sample collection g)type of primary sample; h)measurement procedure, where appropriate; i)examination results reported in SI units, units traceable to SI units, or other applicable units; j)biological reference intervals, clinical decision values k)interpretation of results, where appropriate; NOTE Complete interpretation of results requires the context of clinical information that may not be available to the laboratory. l)other comments such as cautionary or explanatory notes(e.g. quality or adequacy of the primary sample which may have compromised the result, results/interpretations from referral laboratories, use of developmental procedure); m)identification of examinations undertaken as part of a research or development programme and for which no specific claims on measurement performance are available; n)identification of the person(s) reviewing the results and authorizing the release of the report(if not contained in the report, readily available when needed); o)date of the report, and time of release(if not contained in the report, readily available when needed); p)page number to total number of pages (e.g. “Page 1 of 5”, “Page 2 of 5”, etc.). |
建議符合方式:
必須創建一個四階表單「檢測結果單」,並將相關審查、傳遞規定,包含時限(turnaround times,TAT)制訂於《檢測及報告產出管理程序》。當無法在 TAT 內發報告時,則引用《不符合事件管理程序》來決定處置方式與記錄。
「檢測結果單」類似於醫療器材的 Labeling,可讓臨床醫師決定到底要多相信這個 LDT 的檢測結果。
就算(你自認)都符合《LDTs 查核基準》5.5.3 章節規定,在審查過程中,還是很可能會非 · 常 · 多 · 次地被要求修改。(是的,不會一次告訴你要改什麼,會擠牙膏式地慢.慢.告.訴.你。)
看到第(m)項:「作為研究或發展方案一部份檢測的識別,且無法取得其量測性能的特定宣告。」意思是,所以就算不知道「量測性能」,只要標示清楚,也是可以取得食藥署的 LDTs 實驗室的認證喔?
檢測結果的發放
實驗室應有檢測結果發放的相關規劃設計;另實驗室對於檢測結果之修改,應建立程序與管理機制。
| LDTs 查核基準 | ISO 15189:2012,5.9 |
|---|---|
| 5.6 檢測結果的發放 5.6.1 概述 – 實驗室應建立檢測結果發放的文件化程序,包括詳細至,誰可以發放結果與發放給誰。 – 此程序應確保符合以下條件 : a)當接收的原始樣本品質不適合檢測,或可能影響結果時,應於檢測結果單中註明。 b)當檢測結果落於所設定的「警告」或「危急」區間時: – 醫師(或其他已授權健康專業人員)立即獲得通知,(此包括接收樣本並送交受委託實驗室檢測的結果)(見 4.2); – 維持採行行動的紀錄,包括記錄日期、時間、負責的實驗室人員、被通知與檢測結果被傳達的人、及通知過程遭遇的任何困難。 c)結果清晰易讀,轉錄無錯誤,並發放給已授權接受與使用此資訊的人員; d)當傳送結果為臨時結果,最終檢測結果單仍需發送給申請者。 e)以電話或電子式途徑傳送結果,應有程序確保僅傳達到已授權人員。提供口頭結果後應接續提供文字化的檢測結果單。所有口頭提供結果應予以記錄。 5.6.2 檢測結果的自動篩選與發放 – 若實驗室實施檢測結果的自動篩選與發放系統,應建立文件化的程序以確保: a)自動篩選與發放檢測結果的準則應予以明訂、核准、方便提供人員取閱與瞭解; 附註:當實施自動篩選與發放應考量的項目,包括需審查受檢者先前數值的變動與需要實驗室人員介入處理的數值,例如,荒謬、不可能或危急值。 b)準則使用前已確認其可適當運行,並查證其改變後對系統可能的運行影響; c)有顯示樣本存在干擾(例如,溶血、黃疸、脂血)而可能改變檢測結果的程序; d)有從儀器之分析警告訊息嵌入自動篩選與發放檢測結果準則的程序,適當時; e)被篩選為自動發放的結果,應於發放前之審查時可以辨識,並包括篩選的日期與時間; f)有自動篩選與發放檢測結果的快速暫時終止程序。 | 5.9 Release of results 5.9.1 General The laboratory shall establish documented procedures for the release of examination results, including details of who may release results and to whom. The procedures shall ensure that the following conditions are met. a)When the quality of the primary sample received is unsuitable for examination, or could have compromised the result, this is indicated in the report. b)When examination results fall within established “alert” or “critical” intervals: – a physician(or other authorized health professional) is notified immediately [this includes results received on samples sent to referral laboratories for examination(see 4.5)]; – records are maintained of actions taken that document date, time, responsible laboratory staff member, person notified and examination results conveyed, and any difficulties encountered in notifications. c)Results are legible, without mistakes in transcription, and reported to persons authorized to receive and use the information. d)When results are transmitted as an interim report, the final report is always forwarded to the requester. e)There are processes for ensuring that results distributed by telephone or electronic means reach only authorized recipients. Results provided orally shall be followed by a written report. There shall be a record of all oral results provided. NOTE 2 Results of laboratory examinations that have been separated from all patient identification may be used for such purposes as epidemiology, demography or other statistical analyses. See also 4.9. 5.9.2 Automated selection and reporting of results If the laboratory implements a system for automated selection and reporting of results, it shall establish a documented procedure to ensure that: a)the criteria for automated selection and reporting are defined, approved, readily available and understood by the staff; NOTE Items for consideration when implementing automated selection and reporting include changes from previous patient values that require review and values that require intervention by laboratory personnel, such as absurd, unlikely or critical values. b)the criteria are validated for proper functioning before use and verified after changes to the system that might affect their functioning; c)there is a process for indicating the presence of sample interferences(e.g. haemolysis, icterus, lipaemia) that may alter the results of the examination; d)there is a process for incorporating analytical warning messages from the instruments into the automated selection and reporting criteria, when appropriate; e)results selected for automated reporting shall be identifiable at the time of review before release and include date and time of selection; f)there is a process for rapid suspension of automated selection and reporting. |
建議符合方式:
這部分的規定可以全部規範於《檢測及報告產出管理程序》。如果有電子化的檢測結果自動篩選與發放,則可以依循《設備軟體與資訊系統維護程序》,在正式運作前確認相關資訊系統是否可適當運作。
有任何變動,也可利用《變更管理程序》來確認所造成的影響,以及所需要執行的工作是否符合要求。
| LDTs 查核基準 | ISO 15189:2012,5.9 |
|---|---|
| 5.6.3 修改的檢測結果單 – 當原始檢測結果單被修改時,應有修改的相關文字化說明,因此: a)已修改檢測結果單應明確識別修改版,並包括索引至原始檢測結果單的日期與識別; b)給使用者明瞭的修改提醒; c)已修改紀錄顯示更改時間、日期以及負責更改人員姓名; d)修改後,原始登錄的檢測結果單仍能保留在紀錄內。 – 已提供臨床決策的結果經修改後,皆應保留在後續累積檢測結果,並清楚辨識檢測結果單已經修改。 – 若檢測結果單發放系統無法擷取修正、變更或補正,該項紀錄應予以保存。 | 5.9.3 Revised reports When an original report is revised there shall be written instructions regarding the revision so that: a)the revised report is clearly identified as a revision and includes reference to the date b)the user is made aware of the revision; c)the revised record shows the time and date of the change and the name of the person responsible for the change; d)the original report entries remain in the record when revisions are made. Results that have been made available for clinical decision making and revised shall be retained in subsequent cumulative reports and clearly identified as having been revised. When the reporting system cannot capture amendments, changes or alterations, a record of such shall be kept. |
建議符合方式:
這邊的所有規定都可明訂於《檢測及報告產出管理程序》。
實驗室資訊管理
實驗室應有資訊流程管理機制並重視資訊系統管理。
| LDTs 查核基準 | ISO 15189:2012,5.10 |
|---|---|
| 5.7 實驗室資訊管理 5.7.1 概述 – 實驗室為提供符合使用者需求與要求的服務,應可取得必要數據與資訊。 – 實驗室應有文件化的程序,確保檢體資訊機密性可隨時予以維護。 附註:於本查核基準所指的「資訊系統」,包括在電腦化與未電腦化系統內的數據與資訊之管理。與非電腦化系統相比,某些要求可能更適用於電腦化系統。電腦化系統可包括那些整合實驗室設備內運行的系統與採用一般軟體的獨立系統(例如產生、校對、呈現結果及歸檔資訊與檢測結果單之文書處理、試算表及資料庫應用程式 )。 5.7.2 職權與職責 – 實驗室應確保資訊系統的管理之職權與職責已明訂。 – 實驗室應明訂所有使用系統的人員之職權與職責,特別是以下人員: a)取得檢體的數據與資訊; b)輸入檢體數據與檢測結果; c)更改數據或檢測結果; d)授權釋出檢測結果單。 5.7.3 資訊系統管理 – 用於檢測數據與資訊的收集、處理、記錄、呈現結果、儲存或擷取之系統,應: a)導入前供應商已完成確認與實驗室已查證其運行,並在實施前,對系統的任何變更,已被授權、文件化及查證; 附註:確認與查證,包括,若適用時,實驗室資訊系統與其他系統間之介面適當的運行,例如和實驗室儀器、醫院行政系統及初級照護系統等。 b)已文件化與方便已授權使用者取用的文件,包括系統的日常運行; c)防止未經授權取得; d)防止竄改或遺失之保護; e)遵照供應商規格的環境操作,或在未具電腦化系統時,提供保護人工記錄與轉錄準確性的條件。 f)以確保數據與資訊完整性的方式維持,與包括記錄系統故障與其適當的立即與矯正措施; g)遵照國家或國際關於數據保護的要求。 – 意圖從實驗室外部資訊系統(例如,電腦系統、傳真機、電子郵件、網站、個人網際裝置)直接接受資訊,實驗室應就檢測結果、與其有關的資訊與備註(如電子式與由電腦輸出副本有關時)之重製的正確性加以查證。 – 當有新檢測項目或自動化備註已實施時,實驗室應就意圖從實驗室外部資訊系統直接接受資訊之該項變更的重製正確性加以查證。 – 實驗室應有維持服務之文件化應變計畫,以因應發生資訊系統故障或當機事件影響實驗室提供服務的能力。 – 當資訊系統於外部場所或由分包給替代的提供者加以管理與維持時,實驗室管理階層應有職責以確保系統提供者或操作者,遵照本查核基準所有適用的要求。 | 5.10 Laboratory information management 5.10.1 General The laboratory shall have access to the data and information needed to provide a service which meets the needs and requirements of the user. The laboratory shall have a documented procedure to ensure that the confidentiality of patient information is maintained at all times. NOTE In this International Standard, “information systems” includes the management of data and information contained in both computer and non-computerized systems. Some of the requirements may be more applicable to computer systems than to non-computerized systems. Computerized systems can include those integral to the functioning of laboratory equipment and stand alone systems using generic software, such as word processing, spreadsheet and database applications that generate, collate, report and archive patient information and reports. 5.10.2 Authorities and responsibilities The laboratory shall ensure that the authorities and responsibilities for the management of the information system are defined, including the maintenance and modification to the information system(s) that may affect patient care. The laboratory shall define the authorities and responsibilities of all personnel who use the system, in particular those who: a)access patient data and information; b)enter c)change d)authorize the release of examination results and reports. 5.10.3 Information system management The system(s) used for the collection, processing, recording, reporting, storage or retrieval of examination data and information shall be: a)validated by the supplier and verified for functioning by the laboratory before introduction, with any changes to the system authorized, documented and verified before implementation; NOTE Validation and verification include, where applicable, the proper functioning of interfaces between the laboratory information system and other systems such as with laboratory instrumentation, hospital patient administration systems and systems in primary care. b)documented, and the documentation, including that for day to day functioning of the system, readily available to authorized users; c)protected from unauthorized access; d)safeguarded against tampering or loss; e)operated in an environment that complies with supplier specifications or, in the case of non-computerized systems, provides conditions which safeguard the accuracy of manual recording and transcription; f)maintained in a manner that ensures the integrity of the data and information and includes the recording of system failures and the appropriate immediate and corrective actions; g)in compliance with national or international requirements regarding data protection. The laboratory shall verify that the results of examinations, associated information and comments are accurately reproduced, electronically and in hard copy where relevant, by the information systems external to the laboratory intended to directly receive the information (e.g. computer systems, fax machines, e-mail, website, personal web devices). When a new examination or automated comments are implemented, the laboratory shall verify that the changes are accurately reproduced by the information systems external to the laboratory intended to directly receive information from the laboratory. The laboratory shall have documented contingency plans to maintain services in the event of failure or downtime in information systems that affects the laboratory’s ability to provide service. When the information system(s) are managed and maintained off-site or subcontracted to an alternative provider, laboratory management shall be responsible for ensuring that the provider or operator of the system complies with all applicable requirements of this International Standard. |
建議符合方式:
就用《設備軟體與資訊系統維護程序》和《應變管理程序》來結束這一回合吧。
8.6 檢測項目確效與驗證
檢測項目確效應提供規格、方法、原始檢測紀錄及檢測結果,以確保檢測方法的可信度。
| LDTs 查核基準 | ISO 15189:2012,5.1.9 |
|---|---|
| 6.1 檢測項目分析確效 6.1.1 對檢測項目確效應有確效計畫書,並納入作業標準(如項目及允收標準等)、標準作業流程(如檢測過程之流程圖及其描述)、規劃(如檢體型態/數量)及檢測結果評估機制(如效能限制)等,並予以文件化。 6.1.2 應依檢測項目特性,評估須執行之檢測項目確效內容並提供規格、方法、原始檢測紀錄及檢測結果相關文件化資料,以確保檢測方法的可信度: (1)準確性(Accuracy) (2)精密度/再現性(Precision/Reproducibility) (3)可報告區間(Reportable Range) (4)閥值確認(Cut-off Value) (5)追溯性(Traceability) 附註:倘有國際標準品可採用,實驗室應追溯至國際標準品;如為標準品應追溯至標準法。如實驗室採自行建立之標準品作為確效依據時,查核員將於現場再次確認該實驗室應執行之方式,必要時與實驗室管理階層溝通其標準品應達可追溯之最高等級。 (6)靈敏度(Sensitivity) (7)特異性(Specificity) (8)干擾性研究(Interference Study) (9)安定性(Stability) | 《LDTs 查核基準》上寫此部分的參考標準是 ISO 15189:2012 的 Sec. 5.1.9。不過,ISO 15189:2012 的 5.1.9 章節是教育訓練章節的「5.1.9 Personnel records」欸!∑( ̄□ ̄;) |
建議符合方式:
把相關規定全都放在《開發、查證及確效管理程序》裡面吧。
| LDTs 查核基準 | ISO 15189:2012 |
|---|---|
| 6.2 醫療機構如有執行驗證之需求時,實驗室應配合醫療機構要求,提供原始檢測紀錄及檢測結果等資料。 | N/A |
建議符合方式:
可以規定在《文件與紀錄管理程序》裡面。

看到這裡,是不是覺得一個頭兩個大有夠麻煩勒?有沒有覺得「為什麼要我做這些無聊的文書工作」呢?平常檢驗、實驗就夠忙了,公司人也很少,幹嘛還要我搞這些?為什麼是我?
如果你的答案都是「YES」,歡迎來找我哦(thebestra01@gmail.com)!
讓我們一起變強吧!(其實是希望你們帶我變強 (*´ω`)人(´ω`*))
